ABSTRACT
Right heart thrombi are detected in approximately 4% of patients with pulmonary embolism. The associated mortality is high, but the optimal strategy remains controversial. We report a case of a large mobile right heart thrombus, complicated by embolism of the right pulmonary artery, which was successfully treated with half-dose alteplase. We briefly review the literature and discuss the therapeutic options, focusing on the advantages of thrombolysis.
LEARNING POINTS
- Mobile right heart thrombi require rapid therapeutic choices between surgical thrombectomy and thrombolysis.
- Half-dose alteplase may be effective, even in the presence of an extensive thrombus burden.
KEYWORDS
Mobile right heart thrombi, pulmonary embolism, half-dose alteplase
CASE DESCRIPTION
An 84-year-old woman presented to the emergency department with a 5-day history of progressive shortness of breath. Her past medical history included arterial hypertension and dyslipidaemia, for which she refused treatment. She had also been diagnosed with anxiety and depression, self-treated with benzodiazepines, and admitted to minimal physical activity and prolonged periods of bed rest.
On examination, the patient appeared distressed, with a respiratory rate of 20 breaths/min; the jugular venous pressure was elevated at 6 cm. Blood pressure was 105/70 mmHg, with a regular pulse of 90 beats per minute, and oxygen saturation was 90% on room air. Heart and lung auscultation was unremarkable, and signs of deep vein thrombosis in the lower limbs were absent.
Methods and Procedures
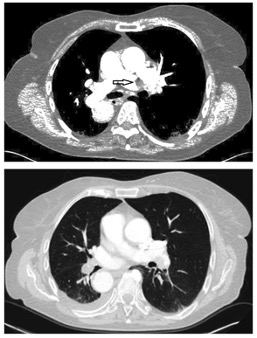
A 12-lead ECG showed sinus rhythm with T-wave inversion in leads V3–V6. Arterial blood gas analysis demonstrated O2 and CO2 partial pressures of 58.2 mmHg and 26.3 mmHg, respectively. Blood biochemistry showed elevated D-dimers (>20 μg/ml, reference value <0.5 μg/ml) and troponin I (184 pg/ml, reference value 0–11.6 pg/ml). A CT pulmonary angiogram showed a large thrombus obstructing the right pulmonary artery (Fig. 1, top).
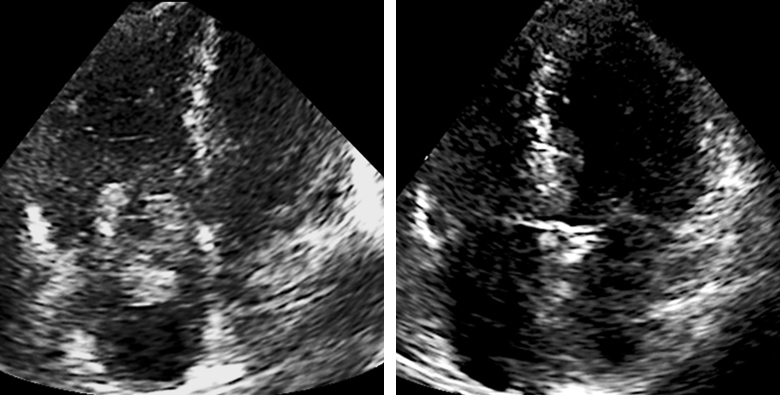
Transthoracic echocardiography revealed an extensive (4.0×2.9 cm) thrombus extending from the right atrium and prolapsing into the right ventricle (Fig. 2, left, Video 1), which was dilated and hypokinetic. Left ventricular systolic function was normal, but there was systolic flattening of the interventricular septum, with an estimated pulmonary artery systolic pressure of 60 mmHg. The inferior vena cava was dilated with minimal respiratory variation.
Treatment and outcome
After the patient was admitted to the coronary care unit, the treatment options were discussed with the patient and her family; it was felt that the risk/benefit balance favoured thrombolysis over surgical thrombectomy, despite the large thrombus size. In case of treatment failure, percutaneous thrombectomy was contemplated, prompting the insertion of a femoral venous sheath.
After a 10 mg bolus, 40 mg of alteplase were administered intravenously over 2 hours, while an echocardiogram was obtained every 30 min. At 90 min, complete thrombus resolution was observed (Fig. 2, right), and fibrinolytic therapy was discontinued 30 min thereafter. Unfractionated heparin was commenced, with dose adjustment guided by the activated partial thromboplastin time (targeting twice the upper reference values).
After thrombolysis, the patient was asymptomatic. Arterial blood gas analysis showed haemoglobin oxygen saturation of 96.7%, with O2 and CO2 partial pressures of 86.8 mmHg and 25.5 mmHg, respectively. A CT pulmonary angiogram revealed complete resolution of the pulmonary embolus (Fig. 1, bottom), while right ventricular dimensions and function on echocardiography, as well as pulmonary artery systolic pressure, normalized. No thrombi were detected on venography of the lower limbs, and thorough investigation for malignancy was negative.
Prolonged (18 days) in-hospital observation was uneventful, during which heparin was substituted for rivaroxaban 15 mg twice daily; 3 weeks after discharge, the dosage of rivaroxaban was reduced to 20 mg once daily. At 6-month follow-up, the patient was asymptomatic and the echocardiogram remained normal.
Figure1. CT scan showing obstruction of the right pulmonary artery (arrow, top panel), with restoration of patency after treatment (bottom panel)
Figure 2. Transthoracic echocardiogram (four-chamber view) showing a large thrombus across the tricuspid valve (left panel), resolving after treatment (right panel)
Video 1 (click to enlarge)
Video 1. Transthoracic echocardiogram (four-chamber view) showing a large mobile thrombus moving across the tricuspid valve.
DISCUSSION and LITERATURE REVIEW
Floating right heart thrombi are rare, but the associated mortality is high if they are left untreated [1]. As in our case, emboli in pulmonary artery branches are invariably present at the time of diagnosis [2]. Despite haemodynamic stability, our patient was thought to be at high risk, due to the presence of right ventricular dysfunction [2]. There is general consensus that large, mobile thrombi, as in our case, are more likely to cause a massive pulmonary embolism, although the exact thrombus characteristics signalling such risk are still debated [3].
The optimal treatment of right heart thrombi remains unclear, as there are no randomized studies, whereas limited experience exists with catheter-directed thrombectomy. Most available evidence comes from two retrospective case series [4, 5] and one prospective registry [6]. Of 177 cases of right heart thrombi in the first series (reported from 1966 through 2000), mortality rates associated with anticoagulation, surgical thrombectomy and thrombolysis were 28.6%, 23.8% and 11.3%, respectively [4]. A more recent series, analyzing 207 patients (reported from 2006 through 2016), found higher mortality after anticoagulation alone (36.4%) than after surgical thrombectomy (18.0%) or thrombolysis (18.2%) [5]. Lastly, a registry analysis compared the outcome after anticoagulation or thrombolysis [6]; pulmonary embolism-related death rates were 7.8% vs. 4.7% and all-cause mortality was 14% vs. 6.2%, respectively, although these differences failed to reach statistical significance.
Critical evaluation of hitherto published experience indicates that anticoagulation alone is insufficient in cases of mobile right heart thrombi complicated by pulmonary embolism, with therapeutic choices lying between surgical thrombectomy and thrombolysis. However, surgical mortality appears high, especially in haemodynamically unstable patients, while the risk of major bleeding is substantial after thrombolysis[4–6]. Therefore, a reduced dosage of alteplase has been proposed, although its fibrinolytic efficacy may be compromised [7].
In our case, an extensive right heart thrombus and a pulmonary embolus resolved rapidly (within 90 min) after 50 mg of alteplase. The thrombi did not recur during prolonged in-hospital observation and the favourable outcome was sustained at 6-month follow-up. We believe that the experience from our case may be helpful in helping clinicians make therapeutic decisions in patients with right-sided thrombi. If surgical risk is deemed high, reduced-dosage alteplase should be considered, even in cases with a large thrombus burden.