ABSTRACT
Background: Ischaemic stroke can be classified according to its aetiology. In cryptogenic stroke, Lambl’s excrescences should be considered since they can only be detected through transesophageal echocardiography (TEE), which is not routinely performed.
Case description: The authors report the case of a 63-year-old Caucasian man with two ischaemic cerebral events associated with the presence of Lambl’s excrescences in the aortic valve detected with TEE. Switching antiaggregant therapy to anticoagulant therapy allowed the patient to remain asymptomatic throughout a 3-year follow-up.
Conclusion: The lack of protocols for the management of cryptogenic stroke results in a delay in the identification of less frequent causes of stroke, leading to recurrent vascular events, morbidity and loss of functionality. The authors describe a patient who experienced multiple cerebral ischaemic events until the correct diagnosis was made.
LEARNING POINTS
- Lambl’s excrescences are a considered a rare cause of embolic stroke, probably because they are underdiagnosed.
- The pathophysiology is not fully understood, making therapeutic decisions difficult.
- Early recognition and management of this structural valve disease can prevent life-threatening complications.
KEYWORDS
Thrombosis, inferior vena cava syndrome, lumbar pain, nephroblastoma
BACKGROUND
Lambl’s excrescences (LE) are filiform structures encountered in valvular leaflets and associated with cellular damage of the endothelium due to shear stress[1]. The pathological process behind these strands is the deposition of fibrin at the site of valvular closure, which leads to the development of a fibroelastic membrane covered by endothelial tissue[2].
They are hypermobile structures and are considered a source of cardiac emboli through microfragmentation of the strands or formation of microtrombi[1,3,4]. LE are diagnosed with transesophageal echocardiography (TEE). There are few studies and consensus is lacking on the most appropriated management of patients with cryptogenic stroke and LE.
CASE DESCRIPTION
The authors report the case of a 63-year-old Caucasian man with a history of type 2 diabetes, arterial hypertension, and one stroke event and one transient ischaemic attack in the previous year. There was no history of alcohol or tobacco abuse. The first stroke presented with sudden dizziness, nausea and inability to walk. On examination, the patient had altered strength in the right arm and diplopia. The CT scan showed left cortico-subcortical frontal-opercular sequela and a small left thalamic lesion. The aetiological study showed elevated total cholesterol (201 mg/dl), low HDL cholesterol (40 mg/dl), a transthoracic echocardiogram with no relevant findings, and a carotid Doppler ultrasound showing 50–60% stenosis of the left bifurcation, with no signs of haemodynamic compromise. The patient was discharged on anti-platelet therapy (acetylsalicylic acid) due to the small vessel aetiology.
Two weeks later, the patient returned to the emergency room with inability to walk and nausea. The physical examination was compatible with a right lacunar syndrome (motor sensitivity syndrome) and full recovery was seen 2 hours after the beginning of symptoms. The CT scan showed right thalamic hypodensity and the patient was again admitted for aetiological study. The transthoracic echocardiogram was unremarkable and there was no evidence of cardiac arrhythmia or a hypercoagulable state, and carotid ultrasound did not show any new stenotic lesions other than those already known. The patient was discharged home asymptomatic and on clopidogrel.
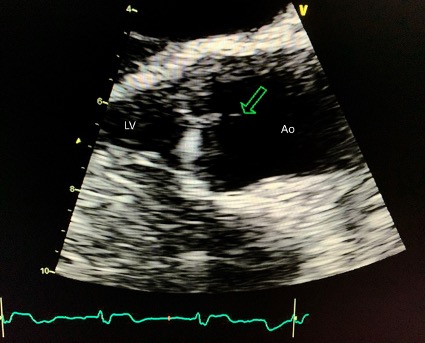
A year later, he was again admitted in the emergency room with complains of occipital headache, blurred vision, inability to walk and dysarthria. The physical examination revealed a partial anterior circulation stroke affecting the left arm and leg, ipsilateral visual field defect and dysarthria. The CT scan showed a new right hypodensity in the cerebral middle artery territory and the patient was admitted. CT angiography did not show occlusion in the great arteries besides the known stenotic lesion in the left carotid. Blood analysis showed hypercholesterolaemia with low HDL cholesterol, A1c haemoglobin of 7.8% and hypertriglyceridemia. There was no evidence of cardiac arrythmia on electrocardiogram or on a 24-hour Holter monitor. TEE was performed and revealed a 4 mm filiform strand adherent to the aortic valve, suggesting a Lambl’s excrescence (Fig. 1). The patient was started on a vitamin K antagonist and began a rehabilitation plan. He was discharged home and on follow-up visits over the next 3 years has remained stable with no evidence of new ischaemic events.
Figure 1. Transesophageal echocardiogram showing a 4 mm strand adherent to the aortic valve in mid-oesophageal long-axis view (arrow)
Ao, aortic root; LV, left ventricle
DISCUSSION
TEE is the exam of choice to detect LE structures[2,4] but is not always included in the primary approach. The main differential diagnoses of LE are fibroelastoma, thrombi and vegetations[2,3]. The natural history of LE has not been fully elucidated but it is considered a source of emboli[4]. The management of LE in clinical practice has not yet been defined. Aziz et al. described the case of a 61-year-old patient with cryptogenic stroke who had three LEs. She underwent surgery and experienced no further events during the first year of follow-up[1]. Wu described the case of a 66-year-old woman who had a stroke associated with a giant LE. Anticoagulation was introduced and she had no recurrences at month 6 [3]. Rhee et al. described the case of a 21-year-old man with stroke due to LE who received antiaggregant therapy and also remained stable for 3 years [4].
Regarding medical treatment, Homma et al. showed no difference between antiaggregant and anticoagulant therapy [2]. It seems reasonable that in recurrent stroke, the therapies should be switched, with surgery remaining an option in giant LE or refractory cases [4]. Therapy should be individualized.
CONCLUSION
Aetiological study of cryptogenic stroke, especially in younger patients, should include ultrasound evaluation with TEE. According to the literature, LE are considered a source of cardioemboli, which should be kept in mind. Although there is little consensus regarding best treatment or pathophysiology (emboli formation vs. microfragmentation), this case shows that treatment should be individualized. Our patient was already under antiaggregant therapy when he experienced the first and second vascular events. However, switching to anticoagulant therapy maintained the patient free from vascular events during 3 years of follow-up.