ABSTRACT
Introduction: Chondrosarcoma is a tumour with a cartilaginous matrix frequently encountered in long bones and the pelvis with rare sinonasal location.
Patient and methods: We report the case of a 25-year-old patient who was referred to us for an extension work-up for sinonasal chondrosarcoma confirmed by anatomopathological examination.
Results: Facial magnetic resonance imaging (MRI) confirmed by a CT scan showed an osteolytic tumour process of the hard palate and walls of the left maxillary sinus that was locally advanced.
Conclusion: The sinonasal location of a chondrosarcoma is rare. Characterized by cross-sectional imaging, confirmation was provided by histological assessment.
LEARNING POINTS
- The sinonasal location of a chondrosarcoma is rare.
- A slow-growing tumour with a cartilage matrix in adults, it is revealed mainly by neurosensorial signs and mass effect in its sinonasal location.
- Radiological characterization includes areas with a weak signal on T1- and T2-weighted images in MRI, not enhanced by gadolinium, corresponding to the cartilage matrix.
KEYWORDS
Chondrosarcoma, cartilaginous matrix, paranasal sinuses
INTRODUCTION
Chondrosarcomas (CSs) are rare, slow-growing, heterogeneous malignant bone tumours that produce a cartilage matrix, preferentially affecting males, and the frequency peak is observed between 40 and 60 years of age. These are the third most common malignancy after myeloma and osteosarcoma, but only 5–10% of CSs are found in the head and neck area. The most common sites of head and neck CSs are the mandible, paranasal sinuses, maxilla, and rarely, the nasal septum. The aim of this report was to describe the CT and MRI aspects of symptomatic sinonasal CS.
CASE DESCRIPTION
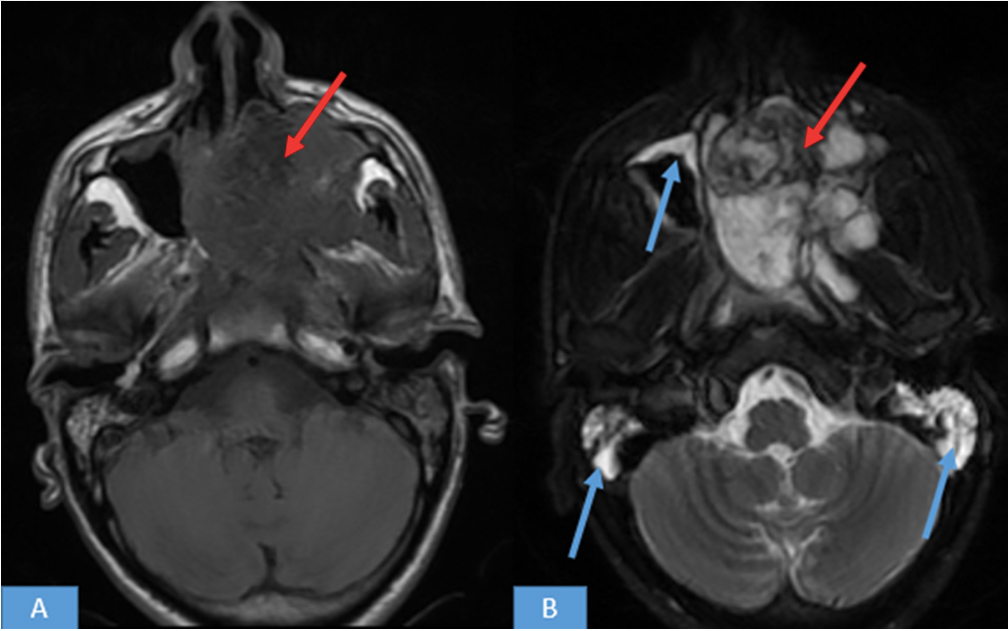
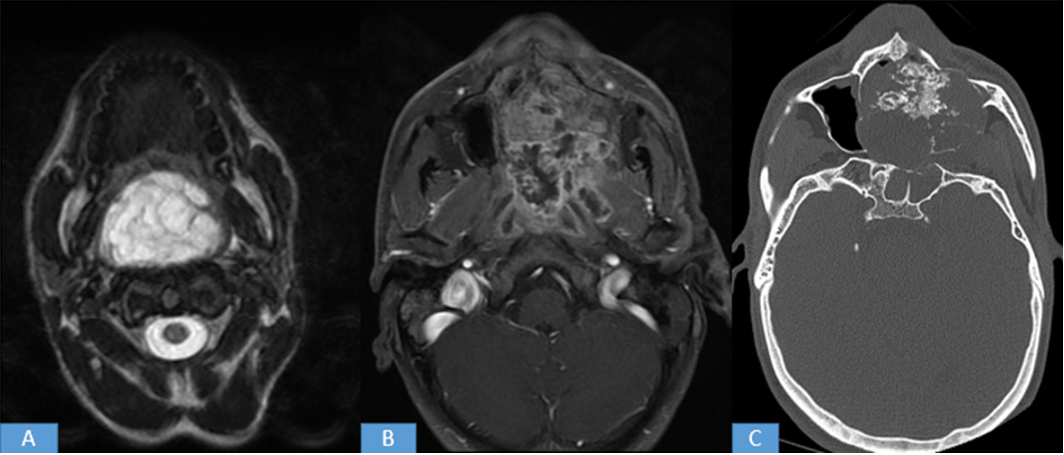
We report a case of a 25-year-old patient complaining of maxillary sinus pain, nasal obstruction, difficulty in swallowing and headache, unaddressed for several years. The exaggeration of symptoms with a feeling of complete nasal obstruction and difficulty swallowing prompted him to consult the Ear, Nose and Throat department. The physical examination found a mass completely filling the nasal cavities. Pathological examination of the biopsies performed under nasofibroscopy concluded that this mass was chondrosarcomatous. The patient was referred to us for MRI as part of the extension work-up. MRI was performed with axial T1 and T2 sequences, a coronal T1 sequence, IDEAL axial and coronal sequences, an axial T2 ganglionic sequence and axial and coronal T1 FAT SAT sequences after injection of gadolinium. It objectified a fairly well-limited tissue sinonasal tumour process, with irregular contours, in heterogeneous isosignal T1, heterogeneous hypersignal T2 (Fig. 1), the site of areas of weak signal in all sequences, it was heterogeneously enhanced after injection of gadolinium (Fig. 2), measured 67.5×52.4 mm and extended over 85 mm.
Figure 1. MRI of the face, axial sequence T1 (A) and T2 (B): left nasal and maxillary tumour process in heterogeneous isosignal T1, heterogeneous hypersignal T2 (red arrows). There was a thickening in the frame of the right maxillary sinus and a filling of the bilateral mastoid cells (blue arrows)
Figure 2. MRI of the face, IDEAL T2 axial sequence (A), T1 axial sequence after injection of gadolinium (B) and axial section on a CT scan of the face in a bone window (C): the tumour process was prolapsed in the nasolabial and oropharyngeal lumen, heterogeneously enhanced after gadolinium injection, with osteolysis of the hard palate and the walls of the maxillary and sphenoid sinuses on the left
This process encompassed the ethmoidal cells and the left maxillary sinus, prolapsed in the nasolabial and oropharyngeal lumen by filling the choanae and the ipsilateral nasal fossa (Fig. 2).
There was replacement of the hypersignal fat of the pterygopalatine cleft, with invasion of the left infratemporal fossa and parapharyngeal space. It came into contact with the floor of the sphenoid sinus with contrast enhancement. There was no detectable sign of endocranial invasion. In addition to the CT scan, bone lysis of the hard palate and the walls of the maxillary sinus was noted (Fig. 2).
DISCUSSION
CS is a malignant tumour that produces a cartilage matrix. It accounts for 20 to 27% of all primary bone sarcomas at any site [1]. CSs mainly appear in long bones and in pelvic bones. Between 5 and 10% of tumours are located in the head and neck area [2]. It is a slow-growing tumour that preferentially affects males and the frequency peak is observed between 40 and 60 years of age [3].
Location in the paranasal sinus system is extremely rare. The main related series of this location is that of Knott et al. [4] where 13 cases were described over a period of 25 years. Other studies report a few cases like Touati et al. [5] with 2 cases, while Krömer et al. [2] and Rowley et al. [6] report one case in each study. The clinical presentation of CS depends primarily on the site affected and the extent of the tumour. In the sinonasal region, nasal obstruction is the most common clinical presentation. Headaches, epistaxis, anosmia, facial pain, visual disturbances and symptoms of cranial nerve damage are other possible symptoms [7].
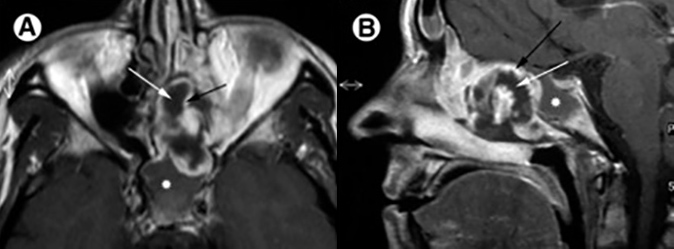
Imaging is based primarily on CT and MRI modalities. CT provides details on bone destruction, including the riddled blade of the ethmoid, the walls of the orbit and the bony palate. Sinonasal CSs tend to expand and reshape the sinonasal cavity. However, the degree of bone erosion increases with the grade of the tumour. Well-differentiated tumours present with punctate cartilaginous calcifications. On MRI, the cartilaginous matrix of CSs presents very low signal intensities on T1- and T2-weighted images (Fig. 3), with homogeneous or heterogeneous enhancement after injection of contrast product. The calcified and ossified areas show a very weak signal on all the sequences [8, 9]. MRI specifies the extension to mainly sensory soft tissues; it differentiates between granulomatous tissue and recurrences during the monitoring of operated CSs.
Figure 3. Chondrosarcoma on MRI. (A and B) Axial and sagittal T1 images after gadolinium injection, showing typical MRI features of low-grade chondrosarcoma with peripheral enhancement (black arrow) and the central cartilage matrix of weak signal in T1 and T2 not enhanced (white arrow). Note the intermediate signal of retention in the obstructed sphenoid sinus (white star)
The diagnosis of CS is made histologically. Conventional CS is the most common form and can be classified into 4 degrees of malignancy based on cell abundance, nuclear polymorphism and the mitotic rate. The other forms are clear cell CS, mesenchymal CS and undifferentiated CS[2]. The differential diagnosis of sinonasal CS includes chondroma, chordoma and chondromyxoid fibroma.
Surgical resection with safety margins is the treatment of choice for sinonasal CS. The role of radiotherapy and chemotherapy is limited and reserved for recurrent or residual diseases. CSs, in general, are known to be radiochemoresistant [7].
CONCLUSION
Sinonasal CS is a very rare, histologically diagnosed, slow-growing, malignant bone tumour with a cartilage matrix. Its radiological exploration is dominated by CT imaging, which can provide details on bone destruction. MRI specifies the extension to mainly sensory soft tissues and is an important imaging tool for postoperative evaluation and monitoring of operated CSs.