ABSTRACT
Patent foramen ovale is a risk factor for systemic embolic events such as cryptogenic stroke. Far less commonly, patent foramen ovale is associated with non-cerebral systemic embolic events. Paradoxical coronary artery embolism is a rare and underdiagnosed cause of acute myocardial infarction. It should be considered in patients presenting with myocardial infarction and an otherwise low-risk profile for atherosclerotic coronary artery disease. We describe a case of paradoxical coronary artery embolism causing ST elevation myocardial infarction. Echocardiography demonstrated patent foramen ovale with a significant shunt. In addition to the treatment of the acute coronary event, patent foramen ovale closure was performed to prevent recurrent paradoxical embolic events.
LEARNING POINTS
- Coronary artery embolism is an established cause of acute coronary syndrome, but paradoxical coronary artery embolism causing myocardial infarction is rare and requires a high degree of clinical suspicion for diagnosis.
- Recognition of this condition is important as it has an influence on management and prognosis. A search for venous thrombosis and underlying prothrombotic conditions should be undertaken.
- Percutaneous device closure of the patent foramen ovale should be considered to prevent future embolic events.
KEYWORDS
Coronary artery, embolism, myocardial infarction, paradoxical embolism
CASE DESCRIPTION
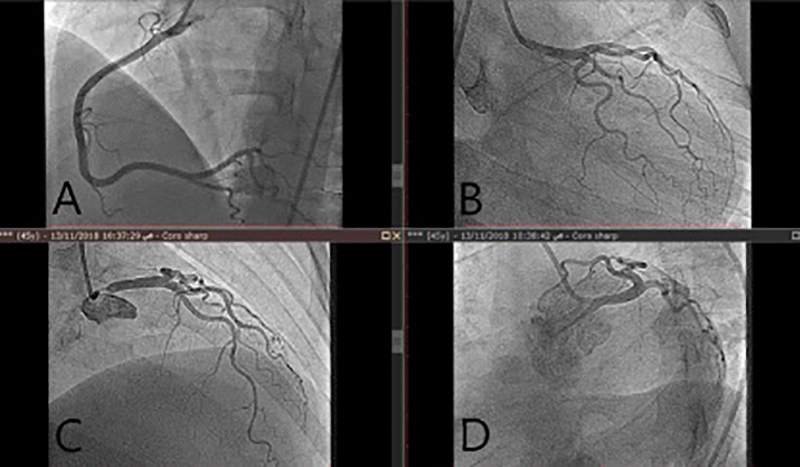
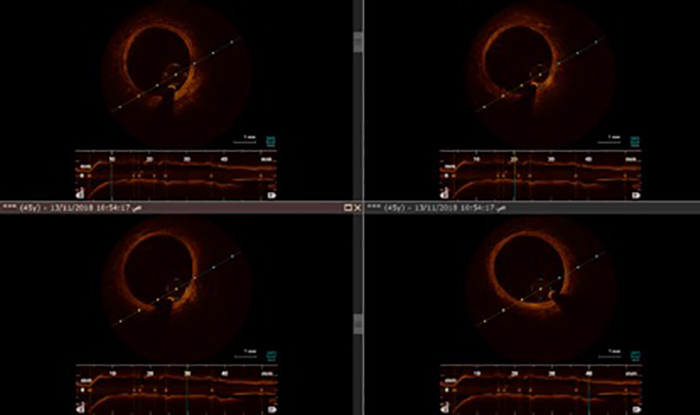
A 46-year-old female presented to the emergency department (ED) complaining of severe chest pain. She had a previous history of type 2 diabetes mellitus controlled by oral medications and a history of menorrhagia treated with oral contraceptive pills (OCPs). She was haemodynamically stable on presentation and her physical examination was unremarkable. A 12-lead electrocardiogram was obtained and revealed inferior ST elevation myocardial infarction (STEMI). She was treated successfully with thrombolysis as she presented to a non-PCI-capable centre. She was then transferred to a PCI-capable centre where she underwent coronary angiography that showed right-dominant circulation with no angiographic evidence of CAD (Fig. 1). Optical coherence tomography (OCT) was performed for the RCA and showed a normal vessel with no evidence of any coronary abnormalities (Fig. 2).
Figure 1. Coronary angiogram showing no significant obstructions in the right (A) or left (B, C and D) coronary artery
Figure 2. OCT showing normal intima, no atherosclerotic plaque
Due to the presentation of acute coronary thrombosis and the absence of plaque or vasospasm, a paradoxical embolism or hypercoagulable state was suspected. An autoimmune and thrombophilia screen was conducted and showed no evidence of hypercoagulability.
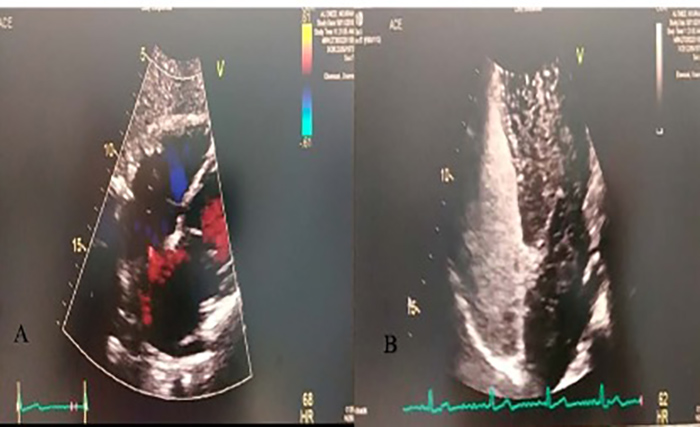
Transthoracic echocardiography (TTE) with a bubble study showed patent foramen ovale (PFO) with a significant right-to-left shunt (Fig. 3). TTE also showed evidence of minimal reduction in the left ventricular ejection fraction (LVEF) and inferolateral hypokinesis.
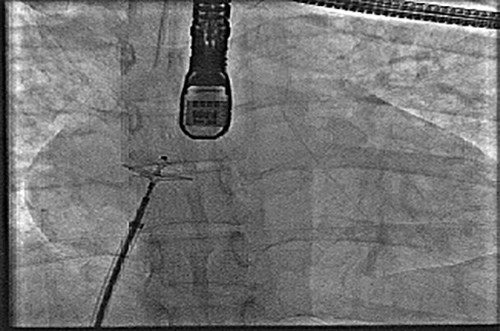
Lower limb Doppler assessment was carried out and showed no evidence of deep venous thrombosis (DVT). The case was discussed at a heart team meeting and the decision was made to offer the patient percutaneous closure of the PFO and the patient was advised against the use of OCPs. Successful PFO closure was performed using an 18 mm Amplatzer occluder with no acute complications (Fig. 4).
Figure 3. TTE: (A) a colour Doppler image showing the PFO shunt; (B) a view showing the positive bubble study for PFO
Figure 4. PFO closure procedure with an Amplatzer occluder
DISCUSSION
PFO is a common abnormality affecting between 20 and 34% of the adult population[1]. For most people it is a benign finding and asymptomatic; however, in some, PFO can enable a paradoxical embolus to transit from the venous to the arterial circulation, causing systemic embolization[2].
The majority of paradoxical coronary artery embolism occurrences are missed clinically and remain undiagnosed. High clinical suspicion is required to make the diagnosis. It is an important diagnosis to make as it has an impact on management and prognosis.
The management of acute coronary syndrome caused by paradoxical coronary artery embolism is similar to that occurring within the setting of atherosclerotic CAD. Manual aspiration thrombectomy can be performed to remove the embolus and PCI can be avoided if the right diagnosis is made. The usual antiplatelet and statin therapy is not required as the underlying diagnosis is not CAD. Beta blockers and ACE inhibitor therapy can be used in cases with evidence of a reduced LVEF. Anticoagulation therapy is used to treat venous thrombosis[3].
In patients presenting with myocardial infarction (MI) and normal coronary arteries, intravascular imaging at the time of coronary angiography can play an important role in reaching the correct diagnosis[4].
A number of recent randomized trials have demonstrated that PFO closure is superior to medical therapy with respect to recurrent systemic embolic events. The early results of the Randomized Evaluation of Recurrent Stroke Comparing PFO Closure to Established Current Standard of Care Treatment (RESPECT) trial did not show benefits of PFO closure; however, recently, an extended follow-up of patients demonstrated that there was a reduction in ischaemic stroke compared with medical therapy[5,6].
The Gore® Septal Occluder device for PFO closure in stroke patients (Gore REDUCE) trial demonstrated a significant reduction in clinical ischaemic stroke when compared with antiplatelet therapy alone[7].
Finally, the Device Closure Versus Medical Therapy for Cryptogenic Stroke Patients With High-Risk Patent Foramen Ovale (DEFENSE-PFO) study showed a reduction in the composite endpoint of stroke, vascular death and Thrombolysis In MI-defined major bleeding at 2 years with PFO closure compared with medical therapy[8].
Although percutaneous device closure has not been studied in paradoxical coronary embolism, closure of PFO would be indicated in a similar manner to that for paradoxical embolic stroke.
CONCLUSION
Paradoxical coronary embolism is a rare cause of acute coronary syndrome. Once suspected, careful imaging including TEE is important for a presumptive diagnosis. In addition to acute management of acute coronary syndrome, PFO closure to prevent recurrent thromboembolism should be considered.