ABSTRACT
Extraintestinal manifestations of Crohn's disease sometimes occur and can present prior to intestinal symptoms. Ocular manifestations of Crohn's disease are considered rare, with orbital myositis an even rarer manifestation with only a handful of cases reported in the literature. We present the case of a young woman who was diagnosed with orbital myositis, which was initially attributed to pseudotumor cerebri after an extensive negative work-up. Months later, the patient presented with haematochezia, and was subsequently diagnosed with Crohn's disease.
LEARNING POINTS
- Orbital myositis is a rare manifestation of inflammatory bowel disease (IBD), and even more rarely is the initial presentation before the development of intestinal luminal disease.
- Orbital myositis is a rare extraintestinal manifestation of Crohn’s disease and mimics thyroid ophthalmopathy. When a thyroid function test is negative, it is important to keep IBD in mind.
KEYWORDS
Crohn’s disease, orbital myositis, extraintestinal manifestations
BACKGROUND
Inflammatory manifestations of Crohn’s disease (CD) that occur outside the gastrointestinal tract, are called extraintestinal manifestations (EIM) and can involve nearly any organ system. Ocular findings are infrequent, with a prevalence of less than 10%, with most being attributed to scleritis episcleritis and uveitis. Orbital myositis (OM) is a very rarely encountered EIM of CD. It is an autoimmune disorder and a subtype of orbital inflammatory syndrome, which is characterized by inflammation of the extraocular muscles. We present a case of OM that was initially attributed to pseudotumor cerebri, only to find out months later that it was an EIM of the patient’s newly diagnosed inflammatory bowel disease (IBD).
CASE DESCRIPTION
A 27-year-old woman with no significant medical history and a family history of CD presented to the hospital with 1 week of progressive left orbital pain increasing with eye movement, with involvement of the left frontotemporal area, associated with blurry vision and increased lacrimation. She was evaluated by the ophthalmologist who ruled out glaucoma and deemed her ophthalmological exam normal. The patient was then sent to the emergency department for neurological evaluation.
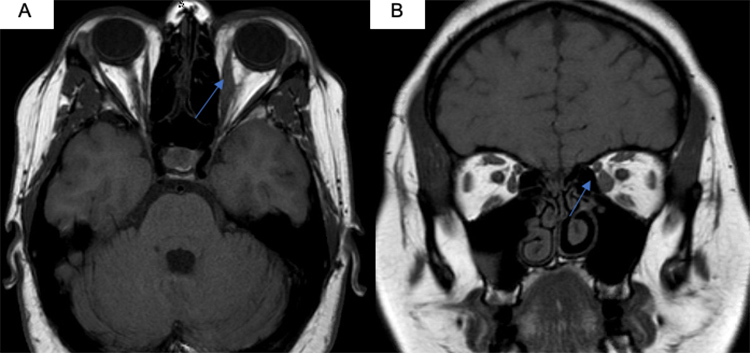
The patient underwent magnetic resonance imaging (MRI) of the brain with and without contrast, which was unremarkable, and an MRI of the orbits with and without contrast (Fig. 1), which was consistent with left medial rectus myositis. The patient was admitted to the neurology department.
Figure 1. Orbital MRI. (A) Axial T1-weighted image showing enlargement and enhancement of the belly of the left medial rectus. (B) Coronal T1-weighted image showing enlargement and enhancement of the belly of the left medial rectus
Initial work-up showed an erythrocyte sedimentation rate (ESR) of 52 mm/h and a C-reactive protein (CRP) of 14 mg/l. However thyroid stimulating hormone (TSH), thyroxine (T4), triiodothyronine (T3), thyroid peroxidase (TPO), thyroid-stimulating immunoglobulin (TSI), Lyme disease serologies, double-stranded deoxyribonucleic acid (ds-DNA), antinuclear antibodies (ANA), anti-synthetase antibodies (Anti-Jo1), anti-neutrophil cytoplasmic autoantibody, anti-Ro (SSA) and anti-La (SSB), anti-Smith antibody, anti-topoisomerase antibodies, and anti-ribonucleoprotein antibodies (anti-RNP) were all within normal limits. The patient then underwent computed tomography of the thorax to evaluate for sarcoidosis, but imaging was unremarkable. A lumbar puncture was performed and was remarkable for an opening pressure of 36 cm, but the cerebrospinal fluid was negative for any infection. The patient was given 1 g of intravenous methylprednisone daily for 3 days, following which her symptoms subsided. Her orbital finding was attributed to idiopathic intracranial hypertension (IIH) and she was discharged on oral acetazolamide 500 mg twice daily and a prednisone taper starting at 60 mg for 9 weeks. She was scheduled for follow-up with the neurologist in 9 weeks, but was lost to follow-up.
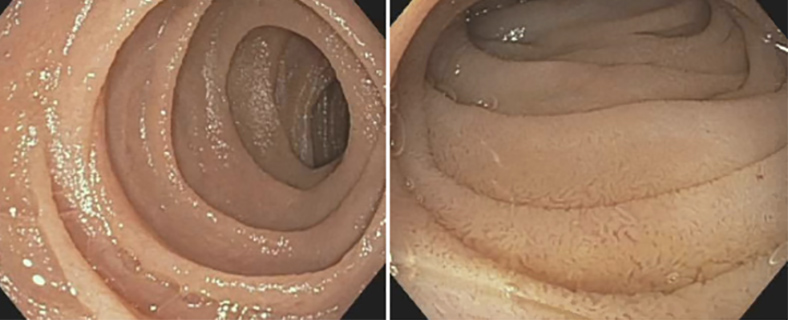
Ten months later, the patient presented to the hospital with worsening pain in her left eye, as well as generalized abdominal pain associated with bright red blood per rectum. The patient stated that she had been having diarrhoea with blood mixed in her stools for the past month. Her neurological and abdominal examinations were unremarkable except for mild tenderness on abdominal palpation. Vital signs were stable. Laboratory results were remarkable for a haemoglobin level of 10.2 g/dl, a mean corpuscular volume (MCV) of 78 fl and a CRP of 56.4 mg/l. A coeliac panel was obtained and was negative. MRI of the orbits was unremarkable, and an abdominal x-ray did not show any intra-abdominal pathology. The gastroenterologists were consulted, and the patient underwent upper endoscopy and colonoscopy which were remarkable for a scalloped mucosa of the duodenum (Fig. 2) as well as nodularity and discoid ulcerations in the terminal ileum (Fig. 3).
Biopsy of the duodenum showed only mild inflammation with preservation of villous architecture and no increase in intraepithelial lymphocytes. Biopsy of the terminal ileum showed expansion of the lamina propria by a lymphoplasmacytic and neutrophilic infiltrate, cryptitis and a rare crypt abscess, but no granuloma or dysplasia was present.
Subsequently, faecal calprotectin and anti-saccharomyces antibody (ASCA) were found to be elevated to 2,900 µg/g and 54.7 units, respectively, and a diagnosis of CD was made. The left rectus myositis previously attributed to IIH was now described as an EIM of CD. The patient was given 1 g of intravenous methylprednisone for 3 days and was safely discharged on an oral prednisone taper with follow-up with the gastroenterologist in 3 weeks for treatment of her CD.
Figure 2. Oesophagogastroduodenoscopy showing scalloped mucosa of the duodenum, an endoscopic feature described in Crohn’s disease
Figure 3. Oesophagogastroduodenoscopy showing nodularity and discoid ulcerations in the terminal ileum consistent with Crohn’s disease
DISCUSSION
EIM are usually seen in 25–40% of IBD cases. Involvement of the skin, eyes, liver and joints are considered the primary and main inflammatory EIM [1]. The pathophysiology behind EIMs and IBD is not clearly understood. Proposed pathogenic autoimmune mechanisms include apparent self-recognition, genetic susceptibility, antigenic display of auto-antigen and immunopathogenic auto-antibodies against organ-specific cellular antigens shared by the colon and extraintestinal organs [1].
Ocular manifestations usually occur in 0.3–5% of all IBD patients, the most common being episcleritis, scleritis and uveitis. OM is a very rare EIM of IBD and its presentation prior to the development of gastrointestinal manifestation is unusual, with only a few cases reported in the literature [2]. It manifests as inflammation of either one or more extraocular muscles and usually presents with mass effects related to the inflammatory process, leading to proptosis, diplopia, orbital swelling, injection and ophthalmoplegia [3].
The differential diagnosis of OM includes trauma, foreign body, infections (Lyme disease, viral infections, orbital abscess, Herpes zoster and syphilis), vasculitis (granulomatosis with polyangiitis, polyarthritis nodosa, Kawasaki disease, giant cell arteritis), sarcoidosis, systemic lupus erythematosus, arteriovenous malformations and IBD [4].
Laboratory results ruled out most of these diseases in our patient, however since she did not have any gastrointestinal symptoms on her initial presentation, a work-up for IBD was not done.
This rare manifestation of IBD emulates the more commonly encountered thyroid ophthalmopathy; however, IBD should be considered if all thyroid tests are negative. Thyroid orbitopathy is typically bilateral with retracted lids and has more involvement of the inferior and medial rectus muscle while sparing the tendinous insertions, in contrast to OM associated with CD, which shows a tubular configuration on imaging that reflects involvement of the tendinous insertion [3].
First-line therapy for CD associated OM has traditionally been corticosteroids, with low-dose orbital radiotherapy, methotrexate, cyclosporine and cyclophosphamide as second-line therapies. When refractory, OM responds well to anti-tumour necrosis factor therapy[5]. While the immediate inflammatory phase of OM is frequently responsive to corticosteroids, recurrences may happen once this dose is tapered. Indeed, this is what prompted our patient to present 10 months later to the emergency department with recurrent orbital pain.
It is important to recognize that orbital myositis may be an EIM of Crohn's disease so that the diagnosis can be made and appropriate therapy started. Clinicians should be aware of this rare EIM of CD that can occur in the absence of luminal disease activity.