ABSTRACT
Objectives: Extensive calcinosis in a patient with dermatomyositis is a rare clinical presentation in adults. The aim of this report is to present the clinical and radiographic features of a 25-year-old woman with dermatomyositis and extensive calcinosis.
Case Presentation: A 25-year-old woman with extensive calcinosis on background dermatomyositis is described.
Results: The clinical and radiographic features of the patient were consistent with dermatomyositis complicated by extensive calcinosis in an adult.
Conclusion: Dermatomyositis with extensive calcinosis is a rare clinical presentation in adults.
LEARNING POINTS
- Dermatomyositis (DM) is uncommonly reported in black Africans.
- Calcinosis, although frequently seen in children, is not common in adults with DM.
KEYWORDS
Rheumatology, calcinosis, dermatomyositis
INTRODUCTION
Dermatomyositis (DM) is a connective tissue disease presenting with multisystemic manifestations primarily affecting the musculoskeletal system, skin, heart, lungs and kidneys. It belongs to the group of idiopathic inflammatory myopathies (IIM). Diagnosis is based on the Bohan and Peter classification criteria[1].
DM is mostly seen in children, with few reports of this condition among African children[2,3] or adult black Africans[4], but with some studies among adult African Americans[5,6,7]. Calcinosis while often reported in children[3] is rarely associated with adult DM cases, which are mostly described in case reports[5,8,9,10]. A larger series was seen in a Brazilian study where calcinosis was seen in nine out of a cohort of 139 DM patients[11]. There are no documented reports of calcinosis in adult black African patients with DM. This report describes a Nigerian DM patient presenting with extensive dystrophic calcinosis.
CASE SUMMARY
A 25-year-old Nigerian woman, without previous features of DM, was diagnosed with DM at the age of 21 years at a rheumatology clinic in Lagos, Nigeria. She had presented then with rashes on the chest and arms. She also had marked difficulty in combing her hair and brushing her teeth, as well as ascending stairs and getting up from a sitting position. Physical examination showed erythematous rashes on the chest (Fig. 1) and arms (Fig. 2). She also had Gottron's lesions on the dorsum of the proximal interphalangeal joints (Fig. 3). Muscle power was grade 3 in the proximal muscles of the arms and leg with normal power in the distal muscles as well as a normal tendon reflex. Examination of other systems was essentially normal.
Laboratory investigations showed an erythrocyte sedimentation rate of 121 mm/hr, creatine kinase 337 U/l (15–170) and serum aldolase 9.5 IU/l (1.5–8.1); AST and ALT were within normal limits. Serology for ANA, ENA, dsDNA, Ro/SSA, La/SSB and anti-Jol were all normal. An electromyography (EMG) test, however, showed a myopathic pattern.
Figure 2: Erythematous rash on the patient's arms
Figure 3: Gottron's lesions on the dorsum of the patient's proximal interphalangeal joints
The patient was placed on a high dose of prednisolone (60 mg daily initially), azathioprine (150 mg daily) and methotrexate (15 mg weekly). Prednisolone has since been tapered off and methotrexate discontinued. She has also had physiotherapy. She has done well on these, with muscle power improving to grade 5 in the proximal muscles.
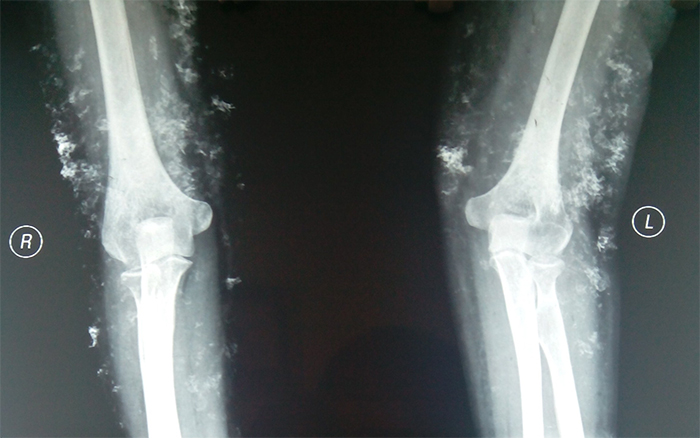
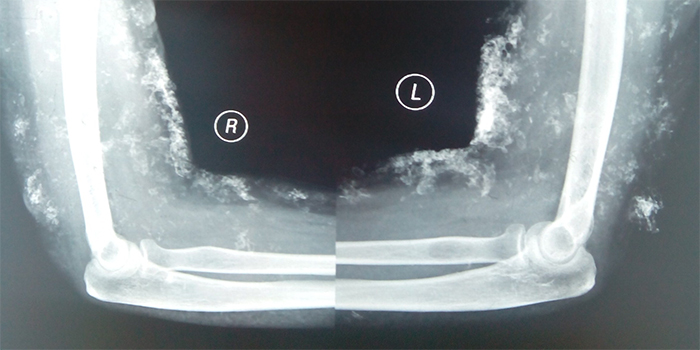
However, the patient presented 5 months ago with nodules around the elbow joints, increasing pain and reduced mobility in the elbow and hip joints. Radiographs of the elbows and pelvis showed extensive calcinosis (Figs. 4 and 5). Investigation showed serum calcium 2.36 mmol/l (2.15–2.65), phosphate 1.12 mmol/l (0.85–1.45) and lactic dehydrogenase 335 U/l (117–256). She has since been started on intravenous pamidronate (30 mg monthly) as well as a non-steroidal anti-inflammatory drug (NSAID).
Figure 4: X-rays of the patient's elbowsjoints
DISCUSSION
The patient had features of DM for 4 years before presenting with nodules and painful elbows and hips. Radiographs of the affected joints showed extensive dystrophic calcinosis in the elbows and pelvis. DM has rarely been reported in black Africans, possibly because of rarity or the few studies carried out. However, there are some reports of this disease among African Americans[5,6,7].
Calcinosis is less frequently reported in adult DM than in childhood DM. For instance, none was seen among cases reported from Nigeria[4], although single cases have been reported elsewhere[5,8,9,10]. The aetiopathogenesis and precipitating factors are poorly understood. It has been suggested that age-dependent factors could influence the risk of developing such ectopic calcifications[12]. Fisler et al.[13] have studied 35 cases of juvenile DM and suggested that factors such as a delay in diagnosis, initiating treatment, prolonged disease duration and increased muscle enzymes may contribute to the development of calcinosis. Pachman et al.[14] have also observed an association between calcinosis and a delay in DM diagnosis.
Different types of calcifications have been reported, such as calcinosis cutis and calcinosis universalis (dermal calcinosis or diffuse interstitial calcinosis)[15]. Dystrophic calcinosis, as seen in our patient, is the most frequently reported. In contrast to other types of calcinosis, it occurs in the presence of normal serum calcium and phosphate levels[16], as in our reported case.
It has been estimated that calcinosis develops a mean of 3–4 years after the onset of DM[17]. Our patient had DM for about 4 years before the development of calcinosis.
Early aggressive treatment of DM remains the best strategy for the prevention of calcinosis. The treatment of established calcinosis is challenging as there is no consistent or standard therapy[18]. Different drugs have been used with variable outcomes. These include colchicine, probenecid, aluminium hydroxide, diltiazem, intravenous immunoglobulins, biphosphonates and even anti-TNFalpha.
Biphosphonate pamidronate has been used in our patient. This is in keeping with other reports where there appears to be complete remission of calcinosis[10,19,20]. The other advantage of intravenous pamidronate over oral biphosphonates is the avoidance of oesophagitis, thereby allowing greater compliance.