ABSTRACT
Paraneoplastic pemphigus arising in association with non-haematological cancers is extremely rare, and there are no reported cases of a patient developing this in the setting of nasopharyngeal carcinoma and only 2 reported cases of patients developing this in response to radiotherapy. Here, we present the case of a patient who developed radiotherapy-associated paraneoplastic pemphigus in the setting of nasopharyngeal carcinoma and who then developed multiple complications.
LEARNING POINTS
- Paraneoplastic pemphigus has a remarkably similar clinical picture to other dermatologic diseases (for example, pemphigus vulgaris), and therefore, it is easy to miss the diagnosis.
- Patients with oral and mucocutaneous lesions refractory to conventional therapy should be worked up for underlying occult malignancy.
- Our case highlights that prompt diagnosis and initiation of immunosuppressive therapy alongside effective management of complications can ensure recovery and survival.
KEYWORDS
Paraneoplastic pemphigus, radiotherapy, nasopharyngeal carcinoma
INTRODUCTION
Paraneoplastic pemphigus (PNP) is an exceedingly rare autoimmune disease that arises in the setting of neoplasias, predominantly of lymphoproliferative origin, such as leukaemia and lymphoma [1]. It is characterized by the presence of autoantibodies against the proteins found in cellular junctions, particularly those found in desmosomes and hemidesmosomes [1]. The diagnosis is made upon correlation of the clinical and histopathological findings which satisfies diagnostic criteria laid out by Anhalt et al. [2], and recently revised by Mimouni et al. [3]. However, given its rarity and variable manifestations, complications and potential multi-organ involvement, the diagnosis and treatment of this condition remains a challenge for physicians.
CASE DESCRIPTION
A 39-year-old male, known smoker presented to a tertiary care hospital with a 1-year history of right-sided headache associated with decreased hearing. Following clinical examination and investigations, MRI was conducted that was suggestive of nasopharyngeal carcinoma, and the suspicion was confirmed upon biopsy.
Treatment was initiated and the patient received 2 cycles of gemcitabine (1,000 mg/m2) and cisplatin (75 mg/m2) over a span of 2 months. In addition, he received 33 fractions of radiation via intensity-modulated radiotherapy over this period. After 6 weeks of radiation, the patient developed a painful rash localized to the irradiated region of the head and neck. This later manifested into multiple erosions and crusted plaques on the right side of the face and neck (Fig. 1), and a well-demarcated, deroofed and crusted plaque on the left cheek. He also developed erosions on the lips and oral mucosa (Fig. 2).
Figure 1. Erosions and crusted plaques could be seen on the right side of the face and neck
Figure 2. Erosions involving the vermillion border of the lip and oral mucosa could be seen
A few months after the initiation of therapy, the patient presented with a new complaint of right-sided chest pain. Work-up was initiated and a CT scan revealed multiple nodules and cavitary lesions in both lungs (Fig. 4). He was started empirically on linezolid and levofloxacin. However, the following week, he developed acute shortness of breath and a chest x-ray revealed a pneumothorax on the right side. A chest tube was inserted and a CT-guided biopsy of the lesion was also conducted, which yielded Gram-positive rods in the infiltrate. The patient was started on meropenem, levofloxacin and voriconazole. He was also tapered of the immunosuppressant therapy in an effort to aid recovery. The condition resolved and the patient was discharged.
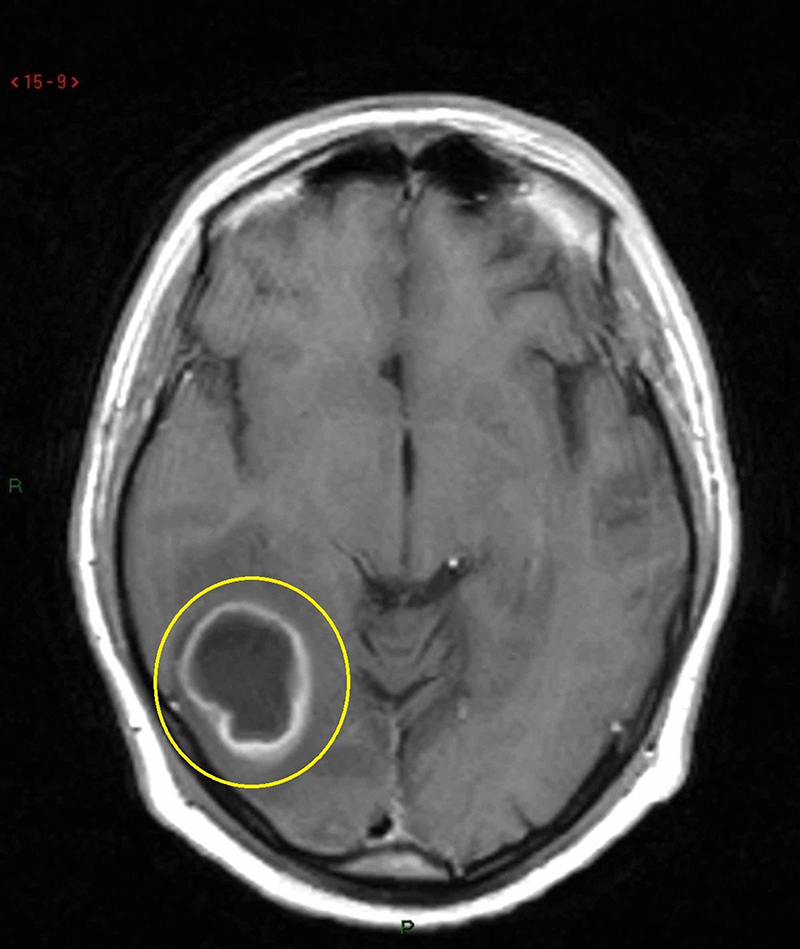
Soon after, however, the patient developed new complaints of severe right-sided headaches, along with episodic blurring of vision in the left eye. MRI was performed and a lesion was identified in the right temporo-occipital region (Fig. 5), which was suspected to be a brain abscess, and antibiotic treatment was initiated. However, the lesion grew rapidly in size and during this period the patient’s complaints worsened. Awake craniotomy was carried out and the abscess was removed. Culture yielded the growth of Nocardia asteroides and the patient was started on trimethoprim-sulfamethoxazole and imipenem. Due to regrowth of the abscess, the antibiotic was changed from imipenem to ceftriaxone. MRI performed 6 weeks later showed a reduction in the size of the abscess with significant clinical improvement.
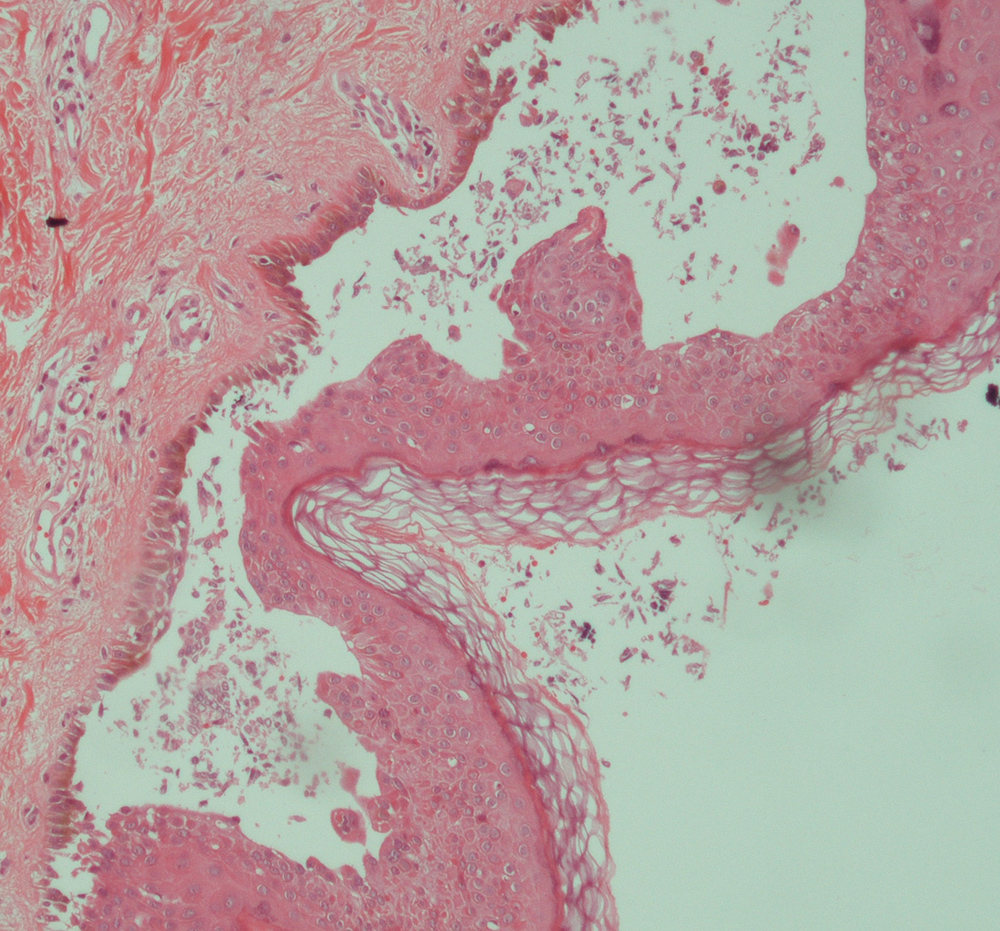
Figure 3. Histology assessment showing acantholysis and keratinocyte apoptosis
Figure 4. CT scan of the lungs showing a cavitating lesion in the left upper lobe (arrow)
Figure 5. T1 MRI showing a cavitating ring-enhancing lesion in the temporo- occipital region with surrounding oedema and mass effect
DISCUSSION
PNP is an extremely rare autoimmune condition first described by Anhalt et al. in 1990 [2]. It occurs in the setting of an underlying malignancy, predominantly of lymphoproliferative origin, but there have been reports of PNP in association with sarcoma, thymoma and other visceral malignancies [1]. However, extensive review of the literature returned no cases of PNP in association with nasopharyngeal carcinoma and only 2 cases where the disease occurred directly in the region of radiation therapy [4, 5], making this case unique.
In most cases, oral and skin lesions are the earliest manifestations of the disease [1]. In fact, these lesions may represent the sole manifestation. However, the clinical features are extremely polymorphous, which may be explained by the presence of different autoantibodies in different presentations of the disease [1].
The lesions involve the vermillion border of the lips and ulceration is present throughout the entire mucosal surface, along with a painful stomatitis. Skin lesions usually follow the onset of the mucosal lesions [1].
Cutaneous involvement is widespread and may include the skin of the head, neck, torso and the proximal parts of the upper limbs.
Pulmonary manifestations are also a common feature of PNP as it affects the respiratory epithelium of patients in up to 92.8% of cases [1], leading to symptoms of dyspnoea, development of obstructive lung disease and characteristically, bronchiolitis obliterans [1].
The differential diagnosis of the disease includes other skin conditions such as pemphigus vulgaris, bullous pemphigoid, erythema multiforme and graft versus host disease, amongst others. In addition, the oral manifestations of the disease can resemble many diseases of the mouth, and as such, a thorough otolaryngologic examination is advisable to rule out other pathologies.
In most cases, the detection of a neoplasm precedes the development of PNP [1]. However, PNP may be the first clinical manifestation leading to the diagnosis of a tumour in approximately 30% of cases [1].
While numerous instances of pemphigoid lesions developing in response to radiotherapy have been reported, the majority turn out to be more common entities such as pemphigus vulgaris or bullous pemphigoid. In fact, extensive review of the literature yielded only 2 cases of PNP that were directly triggered by radiation therapy [4, 5]. No cases of a patient developing PNP in the setting of nasopharyngeal carcinoma were found.
The case presented here is therefore unique in 3 ways; firstly, in that the patient developed PNP, on a background of nasopharyngeal carcinoma. Secondly, it manifested only upon initiation of radiotherapy. Lastly, the patient, despite developing extensive complications, managed to recover, defying the extremely high mortality rate in PNP, accepted to be approximately 90% [1].
It therefore serves to highlight that while the diagnosis and management of the disease is a challenge, if carried out promptly, outcomes can be improved. Owing to its rarity and similar presentations of more common diseases, the diagnosis is often missed.
CONCLUSION
Patients presenting with pemphigoid lesions in the setting of an underlying neoplasm should therefore be investigated for PNP. By the same token, patients presenting with oral and skin ulcers refractory to conventional therapy, with no diagnosed neoplasm, should have a thorough work-up conducted in order to rule out any underlying malignancy.