ABSTRACT
Introduction: Exertional heat illness (EHI) is common in hot weather among young athletes, outdoor manual workers and military personnel. EHI can involve multiple organs of the body, including the muscles, kidneys and brain; however, myocardium involvement is infrequent.
Materials and methods: We present the case of a 26-year-old male construction worker who worked outdoors in a hot arid environment. He presented with acute kidney injury and rhabdomyolysis and was diagnosed with EHI. During his hospital stay, he developed complete heart block, and cardiac MRI showed features of myocarditis. Work-up to identify other aetiologies of myocarditis was normal. This case highlights the effects of EHI on the myocardium.
Conclusion: It is important to keep in mind the various effects of EHI on the myocardium. Myocarditis due to EHI is rare, and conduction defects resulting from it might persist, necessitating specialist intervention.
LEARNING POINTS
- Exertional heat illness (EHI) can cause end-organ damage and it is imperative to keep in mind the various effects of EHI on the myocardium.
- Myocarditis due to EHI is rare, and conduction defects resulting from it might persist, requiring specialist intervention.
KEYWORDS
Exertional heat illness, myocarditis, heart block
INTRODUCTION
Exertional heat illness (EHI) encompasses a spectrum of disorders ranging from heat exhaustion and heat injury to heat stroke [1, 2]. Heat injury is defined as EHI with evidence of hyperthermia (a core temperature above 104–105°F or 40–40.5°C) and end-organ damage, in the absence of neurological manifestations. The most common organs involved are the muscles, kidneys and liver, leading to rhabdomyolysis, acute kidney injury (AKI) and acute liver failure, respectively [3]. Heat injury can also affect the cardiovascular system. Ischaemic ECG changes and conduction defects have been reported [3–6]. Reports in the literature of an association between EHI and myocarditis are extremely uncommon. We present a case of myocarditis associated with exertional heat injury to highlight this rare phenomenon.
CASE DESCRIPTION
A 25-year-old man, not known to have any chronic medical illness, presented to the emergency department with a 1-day history of dizziness and 20 episodes of vomiting. The patient had been working outdoors in hot weather. At his worksite, the patient had a high-grade fever (40.2°C), and cooling measures were provided. He was brought by ambulance to the emergency department. Upon arrival, the patient had a temperature of 37.0°C, a regular pulse of 86 beats/min, a respiratory rate of 18/min, and blood pressure of 122/81 mmHg. Physical examination revealed an ill-looking dehydrated man, oriented to time, place and person. A cardiac, respiratory, nervous system and abdominal examination was unremarkable.
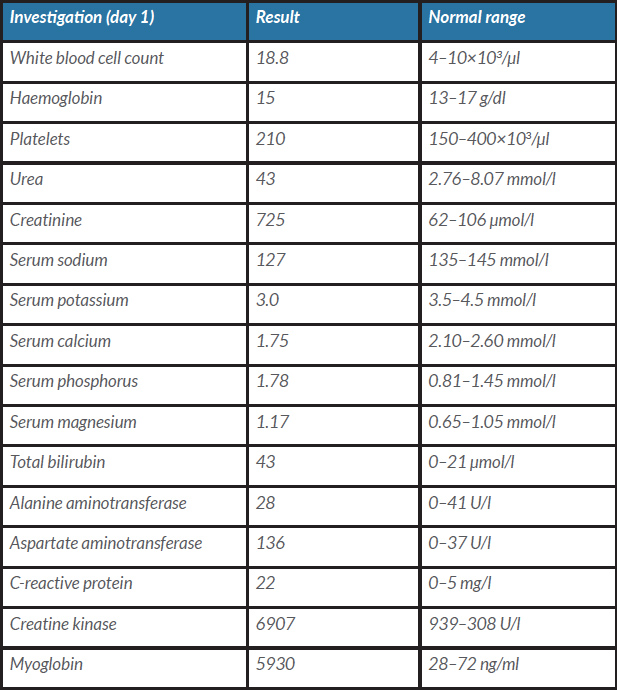
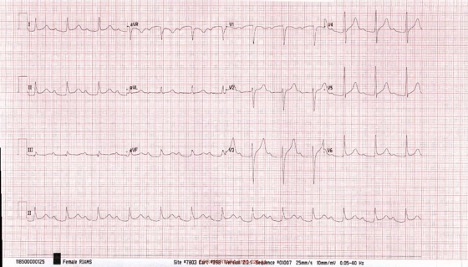
Laboratory results showed raised serum urea, raised creatinine, hyponatremia, hypokalemia, hypocalcemia, hyperphosphatemia, hypermagnesemia, and elevated serum creatine kinase (CK) and myoglobin levels (Table 1). A complete blood count, coagulation profile, autoimmune work-up, and screening for hepatitis B, hepatitis C and HIV were all negative. The chest x-ray was unremarkable. ECG on admission showed a sinus rhythm with a heart rate of 86 beats/min and first-degree heart block (Fig. 1). Non-contrast computed tomography of the kidneys, ureters and bladder did not reveal any signs of obstruction. A working diagnosis of heat injury leading to AKI and rhabdomyolysis was made, and the patient received intravenous fluids. The renal parameters normalized by day 4 of the hospital stay.
Table 1. Initial laboratory results
Figure 1. ECG on admission showing prolongation of PR interval
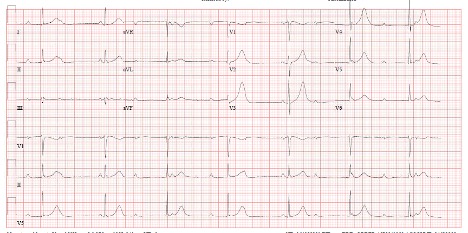
On day 5, the patient developed bradycardia with a heart rate between 35 and 40 beats per minute. However, he did not complain of chest pain, shortness of breath, palpitations or dizziness. All electrolytes were within the normal range. However, ECG showed complete heart block (Fig. 2). Serial troponin levels measured 8 hours apart did not reveal a rising troponin level (781 ng/l and 709.3 ng/l). The echocardiogram showed an ejection fraction of 54% with regional wall motion abnormalities. Coronary angiography showed a calcium score of 0 with no evidence of coronary artery disease. MRI of the heart showed a left ventricular ejection fraction of 66% and myocardial oedema in the basal-to-mid anterior and inferoseptal segments suggestive of myocarditis (Fig. 3). The viral and autoimmune panel was negative. A decision was taken to implant a dual-chamber pacemaker. Following pacemaker implantation, the patient did well, and the rest of the hospital course was uncomplicated. He was discharged and continues to attend for follow-up in the cardiology outpatient clinic.
Figure 2. ECG showing Kadima atrio-ventricular dissociation and supra-Hisian complete heart block
Figure 3. MRI of the heart showing subepicardial basal to mid inferoseptal and inferolateral late gadolinium enhancement of the myocardium along with myocardial oedema consistent with myocarditis
DISCUSSION
EHI includes heat exhaustion, heat injury and heatstroke. Heat exhaustion involves a rise in core body temperature above 38.3°C without end-organ damage or neurological involvement. Heat injury is hyperthermia with end-organ damage and sparing of the neurological system. Heatstroke is a hyperthermia-induced systemic inflammatory response resulting in multi-organ dysfunction. Encephalopathy is a crucial feature of heatstroke [7]. The mainstay of EHI treatment is rapid cooling and administration of intravenous fluids. Ice packing, ice water emersion and evaporative cooling are some non-invasive methods of lowering core body temperature. Invasive methods of cooling include peritoneal, gastric and bladder lavage [8].
EHI can cause various cardiac manifestations. It can manifest as acute myocardial infarction, non-specific ECG changes or Takotsubo cardiomyopathy, and can even lead to cardiac arrest [3, 5, 8–10]. Most of the changes are transient and resolve with the resolution of acute hyperthermia. The pathophysiology of heat-related myocardial injury is poorly understood. Endotoxins and interleukins (IL), including IL-1 and IL-6, are released due to hyperthermia and trigger a systemic inflammatory response leading to end-organ damage [11, 12]. Also, hyperthermia leads to protein denaturation and DNA breakage, causing direct cytotoxicity [13]. Stress-related catecholamine surge is another mechanism leading to cardiomyopathy [14]. Animal models implicate calcium in acute hyperthermic myocardial injury [15, 16].
Myocarditis due to heat-related illness is rarely reported in the literature. One possible explanation for this is under-reporting, as the diagnosis of myocarditis involves cardiac MRI which is not usually performed in patients with EHI. Our patient had first-degree heart block on initial presentation that progressed to a persistent complete heart block. Cardiac MRI was suggestive of myocarditis. An extensive work-up including cardiac enzymes and viral studies for an underlying cause was unrevealing. Thus, the myocarditis and resultant cardiac conduction defects were attributed to heat injury. However, more studies are required to establish the exact extent of association between EHI and myocarditis.