ABSTRACT
Objectives: The aquarium sign is the name given to a large quantity of bubble-like echoes that suggests the presence of hepatic portal venous gas (HPVG). Few studies in the literature have addressed the relationship between the aquarium sign and HPVG. In some cases, HPVG can only be detected using ultrasonography. HPVG can be observed in a variety of conditions, including those that require emergency surgery, such as acute mesenteric ischaemia (AMI). Therefore, it is important to identify the presence of HPVG as soon as possible.
Materials and methods: We report a case of the aquarium sign, where bubble-like echoes flowed from the right atrium towards the right ventricle, which was identified using bedside cardiac ultrasonography as part of a point-of-care ultrasound test.
Results: This aquarium sign finding led to the diagnosis of AMI, which was confirmed using contrast-enhanced computed tomography (CT).
Conclusion: The aquarium sign is a useful finding suggestive of HPVG and mesenteric ischaemia, which can be rapidly and easily observed using bedside cardiac ultrasonography. However, there are very few reports on the aquarium sign. The inability of other more cumbersome diagnostic imaging modalities, such as CT and magnetic resonance imaging, to detect HPVG emphasizes the utility and convenience of detecting the aquarium sign using bedside ultrasonography. This technique can lead to early detection of life-threatening diseases as well as improve the prognosis for patients. The diagnostic implications of the aquarium sign for HPVG are still unclear and require further research.
LEARNING POINTS
- The aquarium sign is a characteristic of hepatic portal venous gas (HPVG), which is often observed in acute mesenteric ischaemia (AMI).
- Owing to the high mortality rate of AMI with HPVG, urgent laparotomy is recommended.
- Bedside ultrasonography can more rapidly and easily detect HPVG than CT imaging, and with a higher degree of sensitivity.
KEYWORDS
Aquarium sign, hepatic portal venous gas, acute mesenteric ischemia, bedside ultrasonography
CASE DESCRIPTION
A 95-year-old man who had been hospitalized for the treatment of adhesive intestinal obstruction complained of acute abdominal pain and vomiting on the 9th day of hospitalization. His medical history included chronic obstructive pulmonary disease, chronic heart failure, vascular dementia, and adhesive intestinal obstruction. His surgical history was significant for cholecystectomy and inguinal hernia repair. At the time of presentation, his medications were aripiprazole, tulobuterol, furosemide, spironolactone, allopurinol and ramelteon. His temperature was 36.6°C, blood pressure was 109/84 mmHg, pulse was 75/min, and oxygen saturation was 93% on ambient air. On examination, he was ill-appearing and his body was warm. Additionally, he presented with skin mottling and diffuse abdominal tenderness with rigidity.
Methods and Procedures
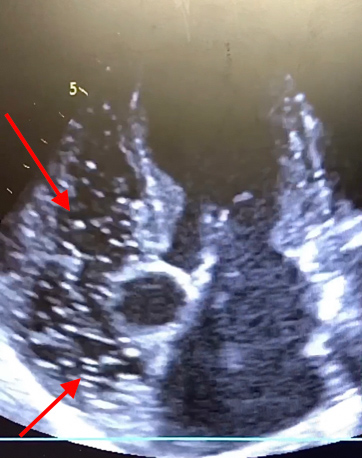
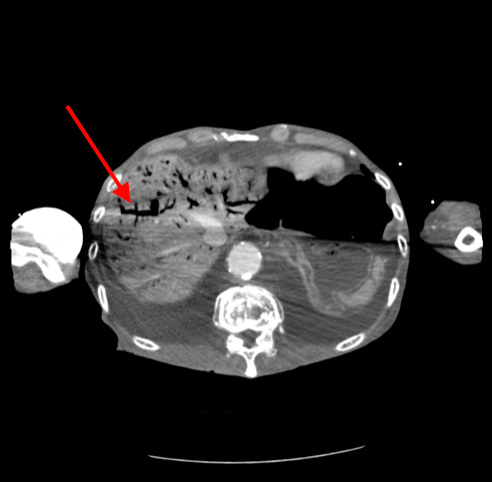
To evaluate this patient, we first performed a point-of-care ultrasound examination. Bedside cardiac ultrasonography revealed a large quantity of bubble-like echoes flowing from the right atrium towards the right ventricle (Fig. 1). This aquarium sign is a characteristic of hepatic portal venous gas (HPVG) flowing through the right chambers of the heart. Arterial blood gas analysis performed with the patient breathing room air revealed the following: pH 7.508, pCO2 21.5 mmHg, HCO3 17.0 mEq/l, pO2 77.9 mmHg, and lactate 3.1 mg/dl. Laboratory findings were as follows: creatinine 0.92 mg/dl, blood urea nitrogen 63.0 mg/dl, sodium 130 mEq/l, potassium 5.6 mEq/l, direct bilirubin 1.2 mg/dl, indirect bilirubin 0.6 mg/dl, aspartate aminotransferase 547 U/l, alanine aminotransferase 411 U/l, alkaline phosphatase 1122 U/l, γ-glutamyl transpeptidase 39 U/l, lactate dehydrogenase 341 U/l, creatine kinase 208 U/l, C-reactive protein 3.06 mg/dl, white blood cells 5800/µl, red blood cells 4.0×106/µl, haemoglobin 13.6 g/dl, and platelets 14.1×104/µl. Next, dynamic computed tomography (CT) revealed massive amounts of HPVG and diffuse, poor enhancement of the bowel wall (Fig. 2). It also showed a patent superior mesenteric artery and ascites. Therefore, the patient was diagnosed with non-occlusive mesenteric ischaemia. Palliative treatment was prescribed because of the patient’s advanced age, but he died later the same day.
Figure 1. Five-chamber view of the cardiac ultrasound showing a large quantity of bubble-like echoes in the right atrium and right ventricle (arrows)
Figure 2. Abdominal contrast-enhanced computed tomography image showing hepatic portal venous gas (arrow)
DISCUSSION
The first adult case of HPVG was reported by Susman and Senturia in 1960 [1]. The exact aetiology of HPVG is unclear, but it can be caused by bowel necrosis, digestive tract dilation, an abscess, ulcerative colitis, a gastric ulcer, endoscopy, Crohn’s disease, or an intraperitoneal tumour [2]. One of the most important differential diagnoses for HPVG is acute mesenteric ischaemia (AMI). The mortality rate of patients with AMI and HPVG is ~75%, and in such cases, urgent laparotomy is recommended [3]. This suggests that the HPVG found in our patient was caused by necrosis and mechanical distension of the bowel wall, which resulted in mucosal disruption. HPVG is often diagnosed using CT[4]. However, in some patients, HPVG can only be detected with ultrasonography [5]. As demonstrated in the diagnostic approach presented here, bedside ultrasonography can be used to rapidly and easily detect HPVG.
To the best of our knowledge, no case reports have been published about the aquarium sign in non-occlusive mesenteric ischaemia, except for some images. The aquarium sign is a useful finding suggestive of HPVG and mesenteric ischaemia, and can be rapidly and easily observed using bedside cardiac ultrasonography. Furthermore, if HPVG which cannot be detected by CT can be identified by bedside ultrasonography, this may result in the earlier detection of life-threatening conditions and, thereby, improve patient prognosis. Because there are very few reports of the aquarium sign, the diagnostic implications of this finding associated with HPVG require further research.