ABSTRACT
Introduction: We tested the MyPrediTM e-platform which is dedicated to the automated, intelligent detection of situations posing a risk of decompensation in geriatric patients.
Objective: The goal was to validate the technological choices, to consolidate the system and to test the robustness of the MyPrediTM e-platform through daily use.
Results: The telemedicine solution took 3,552 measurements for a hospitalized patient during her stay, with an average of 237 measurements per day, and issued 32 alerts, with an average of 2 alerts per day. The main risk was heart failure which generated the most alerts (n=13). The platform had 100% sensitivity for all geriatric risks, and had very satisfactory positive and negative predictive values.
Conclusion: The present experiment validates the technological choices, the tools and the solutions developed.
LEARNING POINTS
- Patients with chronic conditions can be monitored with telemedicine systems to optimise their management, particularly during the COVID-19 pandemic.
- The goal was to validate the technological choices, to consolidate the system and to test the robustness of the MyPrediTM e-platform, through daily use in an elderly patient.
- The present experiment demonstrates the relevance of the technological choices, the tools and the solutions developed.
KEYWORDS
Telemonitoring, geriatric risks, MyPrediTM e-platform, GER-e-TEC study
INTRODUCTION
Telemedicine can be used to optimise the management of elderly patients with chronic conditions. Such systems can decrease morbidity and mortality, reduce re-hospitalization, improve quality of life, and lower medical and economic costs [1].
This was the basis for the “GERIATRICS and e-Technology (GER-e-TEC) study”, which was an experiment involving the use of the smart MyPrediTM e-platform to automatically detect the exacerbation of geriatric syndromes.
METHODS
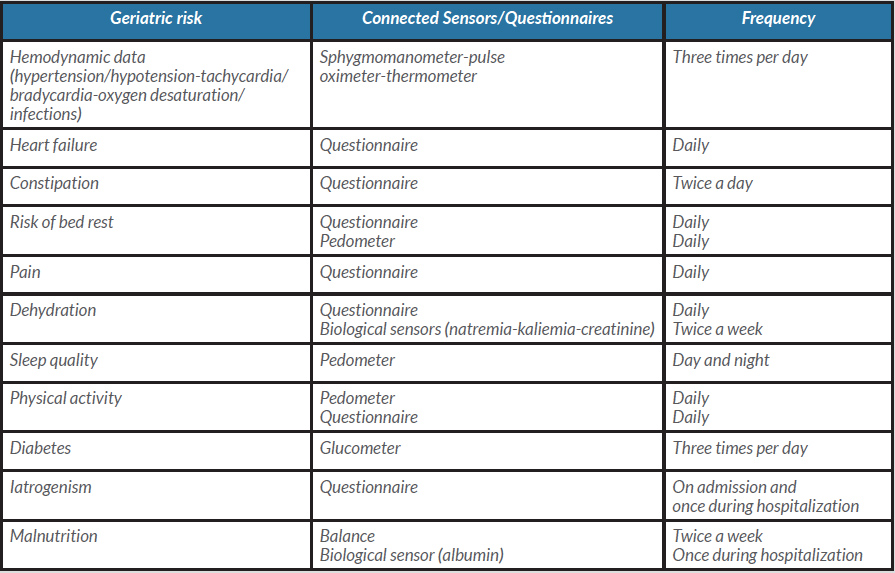
A tablet and connected devices were used to measure patient blood pressure, heart rate, weight, oxygen saturation, capillary blood glucose, temperature and physical activity. The technical characteristics of the sensors are detailed in Table 1. The device has ISO13485 medical certification and CE marking [2].
We gathered information on events common in the geriatric population (falls, constipation, dehydration, confusion, iatrogenism, malnutrition, heart failure, diabetes, infections and bedsores) by means of (a) questionnaires at patient inclusion and during their hospital stay and (b) regular questionnaires during follow-up (Table 2).
Table 1. Remote monitoring of geriatric risks in the GER-e-TEC study
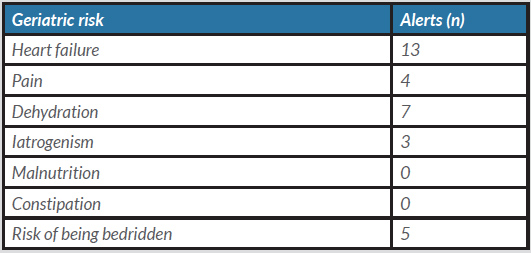
Table 2. Number of alerts and recommendations by geriatric risk
RESULTS
A 73-year-old female patient was admitted to the Emergency Department for the management of bronchial pneumonia. Written consent was obtained for inclusion in the study.
Her medical history included stage 3 COPD (under 1 l of oxygen at home), high blood pressure, dyslipidaemia, an episode of gout and thyroidectomy. Her Charlson's Comorbidity Index score was 4. Usual treatment included L-thyroxine 100 µg daily, candesartan 8 mg once daily, allopurinol 100 mg once daily, atorvastatin 40 mg once daily, bisoprolol 2.5 mg once daily, acetylsalicylic acid 75 mg once daily and furosemide 40 mg once daily. She was independent and lived at home with her daughter with no other assistance.
The patient received telemonitoring surveillance throughout her 17-day hospital stay.
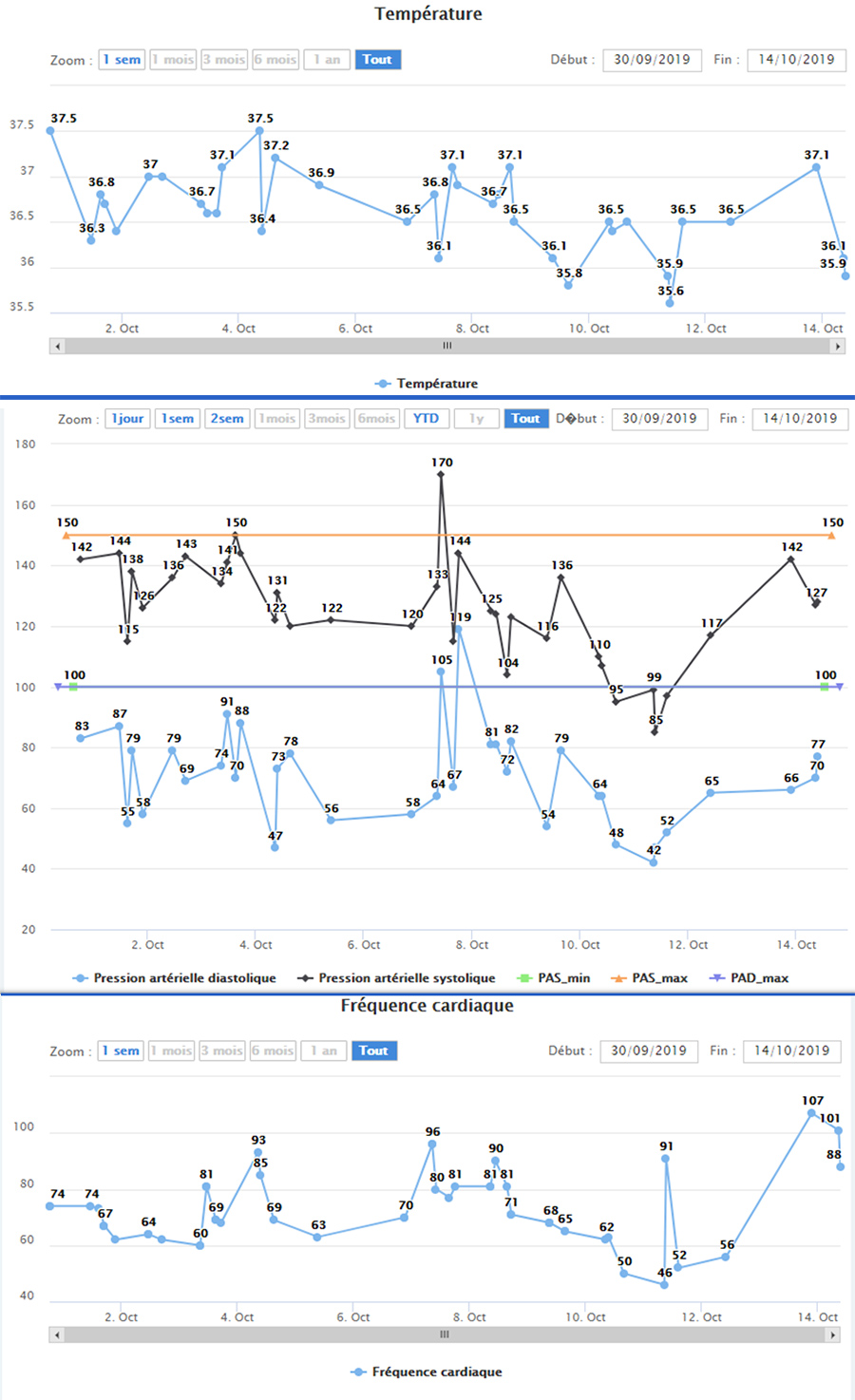
Figure 1 shows some screen shots from the MyPrediTM e-platform remote monitoring system.
Figure 1. Measurements acquired from remote monitoring of the patient’s temperature (top panel), blood pressure (middle panel) and heart rate (bottom panel) during hospitalisation
Mean blood pressure was 104.70±10.16 mmHg, mean heart rate was 72.9±13.1 bpm, and mean oxygen saturation was 94.2±1.4%. Mean activity was 751.6±323.6 steps per day with a median of 806. Mean sleep per day was 455±133.7 min with a median of 512 min. Mean light sleep was 81.8±43 minutes with a median of 87 minutes, and mean deep sleep was 373.2±105.8 min with a median of 398 min. The mean pain VAS (visual analogue scale) was 1.4±2. The mean pain EVS (simple verbal scale) was 0.7±0.8 with a median of 0. Mean weight was 109.7 kg. The mean number of stools was 0.6±0.6 stools per day, and mean temperature was 36.6±0.5°C. The patient answered only two of the nine bedrest questionnaires administered.
The telemedicine system took 3,552 measurements for the patient throughout her hospitalization, with an average of 237 per day, and issued 32 alerts with an average of 3 per day. There were 10 mild alerts, 4 moderate alerts, and 18 severe alerts. Heart failure risk generated the most alerts (n=13; Table 2).
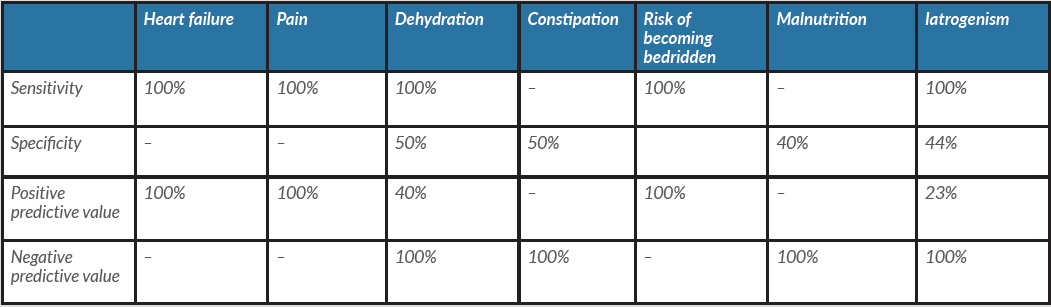
Table 3 shows the sensitivity, specificity, positive predictive values and negative predictive values of the alerts for the criteria studied.
Table 3. Sensitivity, specificity, positive and negative predictive values of alerts from the MyPrediTM e-platform monitoring system
DISCUSSION
Our innovative telemedicine solution enables remote monitoring of geriatric patients through the use of non-intrusive medical sensors that allow the patient's physiological data to be fed back to healthcare professionals. It also includes questionnaires integrated into the MyPrediTM e-platform. Previous work described in the literature has focused primarily on the risk of falling [3, 4] and the monitoring of neuro-psycho-behavioural disorders [5]. Our telemonitoring project will allow us to comprehensively assess elderly patients. The project proposes personalized medical follow-up to prevent acute decompensation via the MyPrediTM e-platform telemonitoring platform, which allows for the early detection of situations posing a risk of deterioration in the patient's health status by sending alerts to healthcare professionals. Daily medical monitoring of patients, based on personalized protocols set up by the medical profession, can be carried out by healthcare teams on the MyPrediTM e-platform using measurements and online questionnaires. When a patient is at risk of deterioration, alerts are sent to a coordinating medical unit so measurements can then be taken.
These results show that the MyPrediTM e-platform telemedicine system automatically and non-intrusively generates alerts related to risk, particularly with regard to pain, immobility and heart failure; it showed high sensitivity and 100% positive predictive values for these three criteria. This experiment also demonstrated that the MyPrediTM e-platform system could detect other risks such as dehydration and iatrogenia. For the practitioner, this means that if no alert is received, then the patient does not require intervention (100% negative predictive value). However, many false alarms can be generated due both to non-compliance with protocol and to likely over-sensitivity of the system.
CONCLUSION
After an experimental phase and following implementation of technological processes on the MyPrediTM e-platform, remote monitoring of 36 patients was carried out between 24 September 2019 and 24 November 2019. The results of this phase of telemonitoring of 10 geriatric risks will be released later.