ABSTRACT
Introduction: Primary malignant mesothelioma of the liver is an extremely rare cancer, with only 16 cases reported in the literature so far. Diagnosis is challenging due to morphological similarity with common liver cancers and the extreme rarity of the condition.
Case description: We present the case of a 70-year-old man who was found to have an incidental liver mass which was diagnosed as primary malignant mesothelioma of the liver.
Conclusion: Our report describes the presentation of this rare liver malignancy and the challenges associated with diagnosis and treatment.
LEARNING POINTS
- Primary malignant mesothelioma of the liver is an extremely rare condition.
- This diagnosis should be considered during the evaluation and treatment of a liver mass.
KEYWORDS
Primary malignant mesothelioma, liver cancer, asbestosis
INTRODUCTION
Primary malignant mesothelioma of the liver is an extremely rare tumour with only 16 previously reported cases. Although asbestos exposure has been linked to 80% of cases of pleural mesothelioma and to 33–50% of cases of peritoneal mesothelioma, an association between asbestos exposure and hepatic mesothelioma has not yet been established. Hepatic mesothelioma is not currently listed in the WHO classification of hepatic tumours [1].
We present a case of primary intrahepatic mesothelioma in a 70-year-old man with asbestos exposure and provide a literature review of the cases reported to date.
CASE DESCRIPTION
A 70-year-old male patient was being followed up at our hospital for pulmonary asbestosis with an annual low-dose CT scan, when an incidental liver mass was detected. His previous CT scan had shown evidence of a stable calcified pleural plaque with no pleural or hepatic lesions. He was completely asymptomatic and showed no signs of jaundice or right upper quadrant tenderness [2].
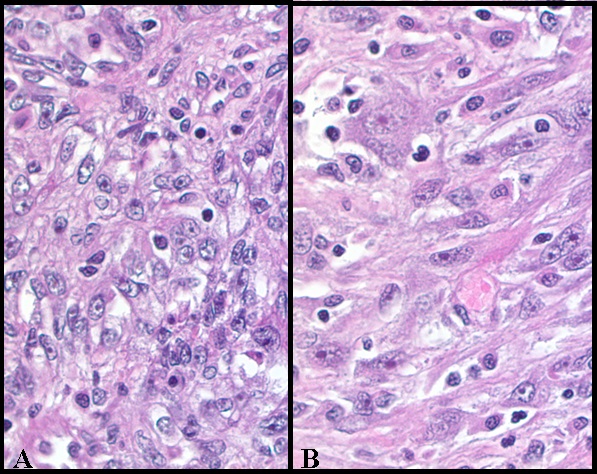
A CT scan of the abdomen with contrast was obtained and showed a well-defined 8 cm mass with heterogenous enhancement involving the right lobe of the liver, predominantly segment VI (Fig. 1). The hepatic vein and portal vein were patent. Since the mass was highly suggestive of malignancy, a detailed work-up was planned. A chest CT scan did not show any evidence of haematogenous metastasis or pleural involvement. Laboratory findings showed liver function tests and alfa fetoprotein (AFP) within normal ranges. The viral markers for hepatitis B and hepatitis C were negative.
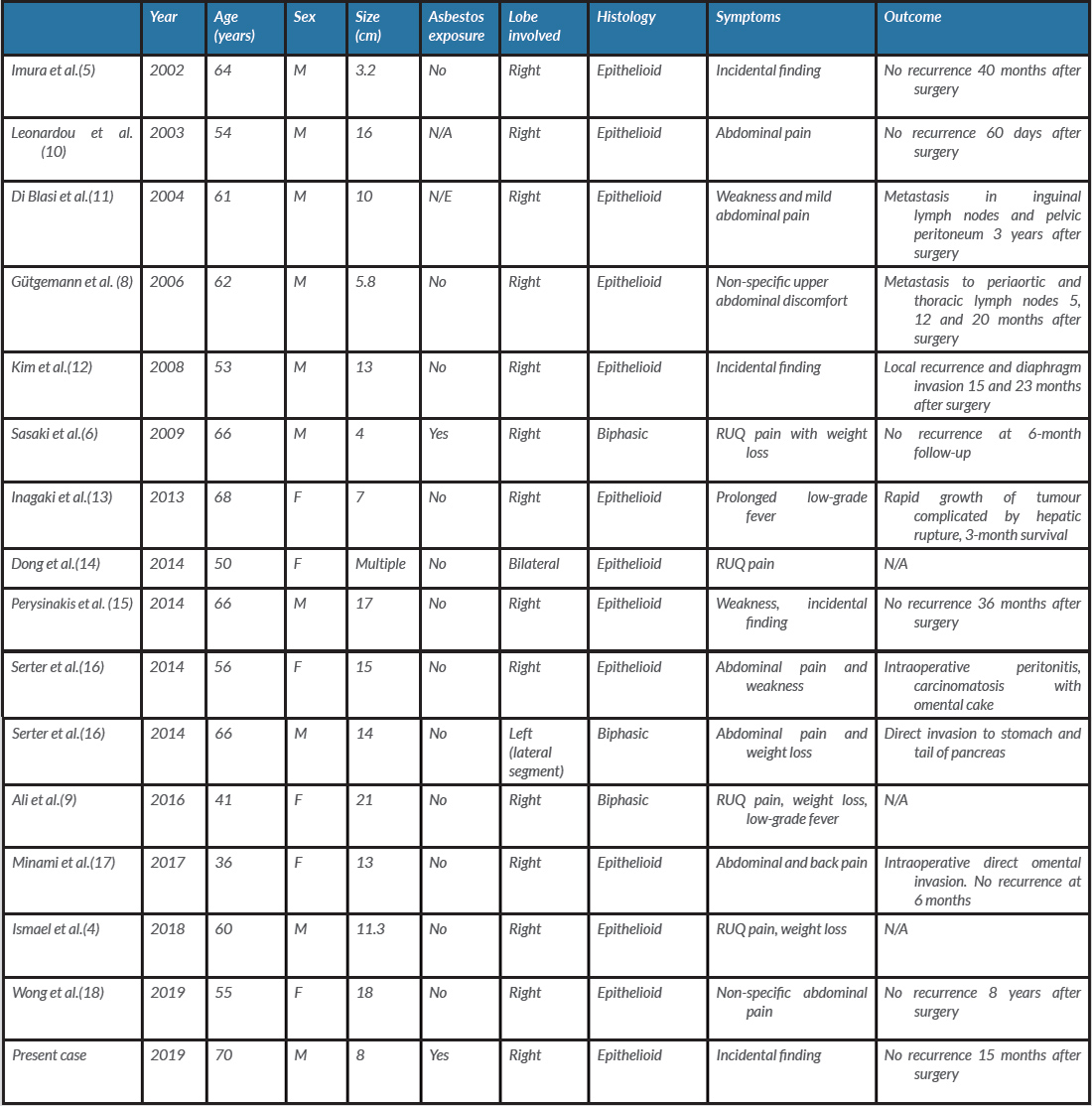
The patient underwent surgical resection with partial hepatectomy (segments V/VI) and cholecystectomy; part of the diaphragm was also resected. Biopsy of the liver mass showed poorly differentiated malignancy with areas of epithelioid and spindle cell differentiation (Fig. 2). Immunohistochemically, tumour cells were positive for keratin AE1/AE3, keratin CAM 5.2, WT1, calretinin, CK20 and D2-40, but negative for CD34, arginase, CK5/6, CK7, ERG, mucicarmine, MOC 31, BerEp4, desmin, S–100, and albumin in situ hybridization. The overall morphology as well as immunohistochemical staining were most consistent with poorly differentiated malignant mesothelioma.
Figure 1. CT scan showing an 8 cm mass in the liver
Figure 2. Tumour cells showing epithelioid (A) and spindle cell
(B) differentiation (H&E stain, ×400)
After surgery, the patient was started on four cycles of pemetrexed and cisplatin as adjuvant therapy, while being monitored for signs of relapse or distant metastasis. So far, there has been no evidence of any new lesions or metastasis, 15 months after surgery.
DISCUSSION
Primary intrahepatic mesothelioma (PIHMM) is an extremely rare tumour with only 16 cases reported in the literature to date [3]. Mesothelial cells form a layer covering Glisson’s capsule but are not present in the liver parenchyma physiologically. Although evidence concerning the origin of liver mesothelioma is unclear, considering the subcapsular location in the majority of cases, many authors have speculated that it originates from Glisson’s capsule and eventually invades the liver [4]. A review of the literature (Table 1) revealed that age at diagnosis ranged from 36 to 70 years (mean: 58 years). Of the diagnosed cases, 62.5% were male and 37.5% were female, showing a slight male preponderance. One case described by Imura et al. was associated with cirrhosis due to hepatitis C infection [5]. Another patient diagnosed with biphasic type mesothelioma had a history of asbestos exposure, making our case the second in the literature to be associated with asbestos exposure. Although there is an association between asbestos and pleural and peritoneal mesothelioma, the association with hepatic mesothelioma is still unclear [6].
Clinically, the majority of patients present with non-specific symptoms such as abdominal pain, weight loss and low-grade fever. In 25% (4/16) of cases, and in our patient, PIHMM was detected as an incidental finding of a localized subcapsular nodular lesion in the right lobe. The average diameter of the tumour was 11 cm (3.2–21 cm). CT scanning with contrast was the imaging modality of choice in all cases. In the majority of cases, it presented as a well-circumscribed tumour with abnormal heterogenous enhancement and areas of necrosis and haemorrhage. Post-contrast enhancement of peripheral serpiginous vascular structure and septal enhancement was also noted.
Histologically, malignant mesothelioma can be divided into three different types: epithelioid, sarcomatoid and biphasic (a mixture of epithelioid and sarcomatoid). Epithelioid is the most common type and can be tubulopapillary or solid and surrounded by either desmoplastic stroma or mixed inflammatory infiltrates.
The clinician should keep in mind other primary and secondary tumours such as hepatocellular carcinoma, cholangiocarcinoma and a metastasized adenocarcinoma when investigating malignant mesothelioma of the liver. Immunohistochemistry helps in the definitive diagnosis of the tumour. A mesothelial origin was proven by positive calretinin, WT-1, cytoplasmic D2-40, cytokeratins, CK AE1/AE3, thrombomodulin staining and negative CD34, Ber-EP4, MOC-31, CEA, AFP and CA-19-9[1,3]. Calretinin, a 29-kDa protein that belongs to a family of calcium-binding proteins, is highly sensitive and specific in diagnosing epithelioid mesothelioma [7, 8].
Treatment is with surgical removal of the tumour and the attached portion of the. Some 37.5% (6/16) of cases reported in the literature showed invasion beyond their original site, metastasis or local recurrence, while 37.5% (6/16) of cases had no recurrence after surgery [4, 9].
CONCLUSION
Primary malignant mesotheliomas are rare tumours detected as well-circumscribed, subcapsular lesions particularly in the right lobe of the liver. Due to the limited number of described cases, the association between asbestos exposure and hepatic mesothelioma is still unclear. Hence, more cases should be reported, while asbestos exposure is kept in mind, to provide a clear understanding. This diagnosis should be considered in the evaluation of liver mass.