ABSTRACT
An association between lymphoma and sarcoidosis was first suggested in 1960. We report a case of sarcoidosis-lymphoma syndrome, which is a diagnostically challenging condition. We conclude that an associated lymphoma should be considered in all patients with suspected sarcoidosis, especially those who do not respond to treatment or who present with persistent haematological abnormalities.Splenomegaly should prompt splenectomy to rule out lymphoma if a less invasive approach has failed to confirm the diagnosis.
LEARNING POINTS
- Clinical consideration should be given to an associated lymphoma in all patients with sarcoidosis, especially those who do not respond to treatment or who present with persistent haematological abnormalities.
- Splenomegaly should raise the possibility of splenectomy to rule out associated lymphoma.
KEYWORDS
Granulomatous diseases, sarcoidosis, lymphoma
INTRODUCTION
The association between lymphoma and sarcoidosis was first suggested in 1960 [1]. Additional cases have since been published without providing a better understanding of this relationship [2–4]. We report one additional case of sarcoidosis-lymphoma syndrome.
CASE DESCRIPTION
Presentation
An 89-year-old woman was admitted for anorexia, weight loss and dyspnoea. Upon admission, she presented bilateral pleural effusion and splenomegaly without adenopathy.
Investigation
A blood test showed a decrease in total proteins and an increase in serum concentrations of calcium (corrected Ca 2.67 mmol/l) associated with normocytic anaemia and hypogammaglobulinemia. Parathyroid hormone (PTH) was <5.5 ng/l, calcitriol was 134 ng/l (normal 29–83) and angiotensin converting enzyme (ACE) 140 U/L.
An x-ray of the thorax confirmed bilateral pleural effusion without mediastinal or parenchymal lesions. The pleural effusion showed a predominance of lymphocytic cells (98%).
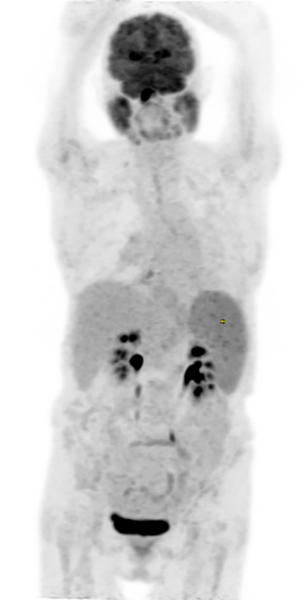
Whole-body 18F-FDG-PET/CT revealed hypermetabolism of the spleen (SUVmax of 5.3). A CT scan of the abdomen and thorax showed bilateral pleural effusion.
Pleural biopsy demonstrated thickening of the pleura, with non-specific chronic pleuritis. Biopsy of the spleen showed non-necrotic granuloma, epithelioid CD 68 cells, and rare B-lymphocyte CD 20+ cells.
Outcome
According to the results of the spleen biopsy, and after exclusion of infectious disease and in the absence of a pathological diagnosis of lymphoma, the presumptive diagnosis of sarcoidosis was proposed. The patient received methylprednisolone 32 mg/day, leading to clinical improvement and normalization of serum calcium.
However, 3 months later, while on methylprednisolone 8 mg/day, the patient’s clinical status declined with weight loss and recurrence of hypercalcemia. Physical examination revealed enlargement of the parotid glands. A second whole-body 18F-FDG PET/CT scan (Fig. 1) revealed the ‘panda sign’ without hypermetabolism in mediastinal lymph nodes but with persistent and stable diffuse splenic hypermetabolism (SUVmax of 4.5).
The patient had no signs of clinical infection and received higher doses of methylprednisolone (16 mg/day) which resulted in clinical improvement. Nevertheless, 2 months later she was admitted to the emergency department with haemophagocytic lymphocytosis leading to her death. Autopsy revealed large B-cell lymphoma with massive invasion of the spleen.
Figure 1. 18F-FDG PET maximum-intensity projections showing diffuse hypermetabolism of the parotid glands (‘panda sign’) and the spleen. The maximum standard uptake value of the spleen was 4.5
DISCUSSION
At the patient’s first admission, the presence of calcitriol-mediated hypercalcemia suggested a diagnosis of tuberculosis [5–8], lymphoma [9] or sarcoidosis. Other rare causes of calcitriol-mediated hypercalcemia [10] were not present. The results of the spleen biopsy were in favour of sarcoidosis, but the post-mortem diagnosis was B-cell lymphoma. So, the question is: was the spleen biopsy misleading or did the patient have sarcoid-lymphoma syndrome? [4, 11]. A multicentre Italian study reported experience with percutaneous ultrasound-guided fine needle aspiration biopsy of the spleen in 398 patients [12]. The overall sensitivity, specificity and accuracy were quite high at 90%, 99% and 91%, respectively. In a recent publication describing a series of 45 spleen biopsies for neoplastic or reactivation conditions, no major complications were reported and minor complications occurred in 3/45 cases (6.7%) [13].
During the first admission, the presumptive diagnosis of sarcoidosis was based on the spleen biopsy (non-necrotic granulomas), increased serum ACE concentration, and calcitriol-mediated hypercalcemia. Nevertheless, the absence of enlarged mediastinal lymph nodes or parenchymal lung lesions and the presence of isolated lymphocytic pleural effusion are uncommon in sarcoidosis. We considered this diagnosis as an exclusion diagnosis since there were no signs of lymphoma or tuberculosis despite the performance of invasive procedures (pleuroscopy with biopsy and spleen biopsy). Because of the patient’s fragile status, a splenectomy was not carried out to confirm the final diagnosis.
During the second admission, the onset of parotid gland enlargement (‘panda sign') was another pointer suggesting the diagnosis of sarcoidosis.
CONCLUSIONS
Clinical consideration should be given to an associated lymphoma in all patients with sarcoidosis, especially those who do not respond to treatment or those who present with persistent haematological abnormalities. This case report suggests splenectomy should be performed in order to rule out lymphoma in such cases.