ABSTRACT
Paratesticular leiomyosarcomas are uncommon malignant tumours that originate from smooth muscle and show aggressive tumour behaviour due to a high incidence of local recurrence and distant metastasis. Orbital metastasis is also rare and associated with a poor prognosis. Clinical suspicion plays an essential role in the diagnosis of orbital leiomyosarcoma because of its uncommon presentation. Comprehensive neuroimaging and histopathological work-up are warranted for definitive diagnosis and management. To date, surgical resection remains the best curative treatment. However, leiomyosarcomas are usually friable and unencapsulated, which makes surgery challenging. Also, whether adjunctive chemotherapy will alter the long-term prognosis remains to be determined. Herein, we report the case of a middle-aged man who presented with proptosis and decreased vision, who was subsequently diagnosed with metastatic orbital leiomyosarcoma from a primary paratesticular tumour. We performed orbital enucleation with negative margins. The patient is currently under systemic pazopanib chemotherapy.
LEARNING POINTS
- Orbital metastasis from paratesticular leiomyosarcoma is rarely encountered and shows aggressive behaviour.
- Clinical suspicion plays an essential role in diagnosing orbital leiomyosarcoma as this is an uncommon and atypical cause of proptosis and can be easily misdiagnosed by physicians.
- Curative surgical treatment should be considered due to the high recurrence rate.
KEYWORDS
Unilateral proptosis, orbital metastasis, paratesticular leiomyosarcoma, ocular enucleation, neuroimaging
INTRODUCTION
Leiomyosarcoma (LMS) is a malignant tumour that originates from smooth muscle and mostly occurs in the uterus, gastrointestinal tract and vascular tissue. Less than 5% of sarcomas and 2% of urological malignancies are soft tissue sarcomas of the genitourinary tract [1]. The incidence of LMS increases with age, peaking in the seventh decade. Well-known predictors of prognosis are tumour grade, stage, histological type and lymph node involvement.
Paratesticular LMS has a high mortality rate with an increased incidence of local recurrence and distant metastasis. The main route of metastasis for LMS of the spermatic cord is haematogenous, and the lungs are the most common site for metastasis [2]. Orbital metastasis from paratesticular LMS is rarely encountered and shows aggressive behaviour. Here we report the case of a 47-year-old male patient who presented with proptosis and was diagnosed with metastatic orbital LMS.
CASE DESCRIPTION
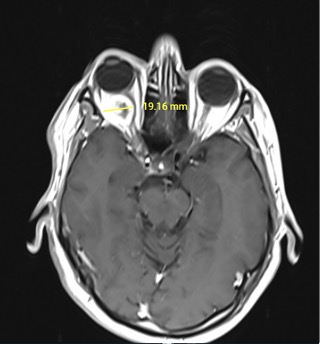
A 47-year-old Caucasian male patient presented with a 4-week history of progressive right-sided painless proptosis and decreased vision of the right eye. He denied any recent injury, headache, lightheadedness or loss of consciousness. His was an active smoker with a 20 pack-year history. Six months previously, he had been diagnosed with grade 2 dedifferentiated paratesticular leiomyosarcoma. Surgery was successful with negative tumour margins. The patient completed six cycles of ifosfamide plus adriamycin adjuvant chemotherapy which resulted in a complete cure. Routine 3-month follow-up with PET/CT after treatment showed no local or distant relapse. On presentation, the patient’s vital signs were within normal limits. His corrected visual acuity was 20/15 in the left eye with minimal light perception in the right eye. The intraocular pressure was 15 mmHg in the left eye and 12 mmHg in the right eye. The pupils were equal in size, and the direct reaction of the right eye was defective with an afferent pupillary defect. Findings by slit-lamp examination were unremarkable, while fundus examination revealed right-sided grade 2 pupil oedema. The rest of the physical examination was within normal limits. Basic laboratory tests and thyroid function tests showed no abnormalities. CT of the head without contrast was unremarkable. Given the patient’s recent history of leiomyosarcoma and sudden onset of unilateral blindness, we suspected tumour metastasis around the right optic nerve. Orbital MRI revealed a 21×18 mm space-occupying, hyperintense heterogenous mass invading the right optic nerve and extending from the right optic canal to the right cavernous sinus (Fig. 1).
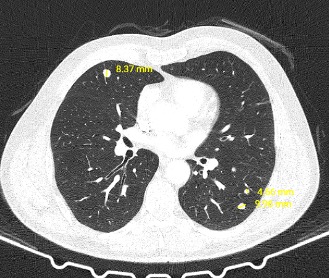
CT of the abdomen and thorax was carried out for staging and revealed multiple metastatic foci in both lungs (Fig. 2). We proceed with right orbital enucleation, and the pathology result confirmed metastatic leiomyosarcoma of the optic nerve with negative surgical margins. Currently, the patient is on systemic pazopanib chemotherapy with routine follow-up.
Figure 1. Orbital MRI revealed a 19.16 mm space-occupying, hyperintense heterogenous mass invading the right optic nerve and extending from the right optic canal to the right cavernous sinus
Figure 2. CT of the abdomen and thorax revealed multiple metastatic foci in both lungs
DISCUSSION
After liposarcoma, LMS is the second most commonly reported malignant paratesticular tumour [3]. LMS constitutes about 24% of spermatic cord tumours, with around 120 cases reported in the literature. The route of metastatic spread of paratesticular LMS is lymphatic, haematogenous and by local invasion. Lymphatic spread may involve the external iliac, hypogastric, common iliac and para-aortic nodes. Haematogenous metastasis primarily targets the lungs. Local invasion may be to the scrotum, inguinal canal or pelvis. Tumour metastatic behaviour is related to the histological grade, site and lymph node involvement.
Paratesticular LMS is an infrequent cause of metastatic lesions to the optic nerve. A search on MEDLINE (2003–2020) using the search terms “paratesticular leiomyosarcoma”, “spermatic cord leiomyosarcoma” and “orbit” yielded two citations, only one of which was a case report of spermatic cord LMS metastasis to the orbit. There were no reports in the English literature before 2003 [4]. Orbital LMS can present with various clinical manifestations such as proptosis, vision loss, eye movement disorders and papilloedema. The condition is difficult to diagnose, but these tumours tend to develop rapidly, which differentiates them from benign tumours.
When orbital tumours are clinically suspected, comprehensive neuroimaging work-up using high-resolution MRI or 18-FDG PET/CT is essential to determine the nature and extent of cancer. Primary orbital LMS are isointense to extraocular muscle tissue and cerebral grey matter on MRI T1-weighted sequences, with notable peripheral rim enhancement. However, metastatic orbital LMS may demonstrate more diffuse enhancement. In our case, the lesion radiographically appeared as a hyperintense heterogenous mass invading the right optic nerve and extending from the right optic canal to the right cavernous sinus.
Histopathological diagnosis is the gold standard diagnostic tool when surgery is acceptable. Coagulation necrosis and high mitotic activity are the main features of LMS. Orbital LMS pathologically can be non-encapsulated, encapsulated and well-demarcated, or partially encapsulated and invading nearby structures [4]. Surgical resection remains the best curative treatment, as these tumours are relatively insensitive to chemotherapy and radiotherapy [5]. However, leiomyosarcomas are usually friable and unencapsulated, which makes surgery challenging. Obtaining a negative surgical margin is associated with decreased recurrence and increased overall survival. In the literature, the utilization of adjuvant chemotherapy and radiotherapy for metastatic disease showed limited benefit [5].
CONCLUSION
Clinical suspicion plays an essential role in the diagnosis of orbital LMS due to its uncommon presentation. Once detected, comprehensive neuroimaging and histopathological work-up is warranted. Curative surgical treatment should be considered due to the high recurrence rate. Also, whether adjunctive chemotherapy alters the long-term prognosis remains to be determined.