ABSTRACT
Erythema nodosum (EN) is an inflammatory condition of the subcutaneous fat and has been reported in patients with haematological malignancies (lymphomas) or solid tumours. Lung cancer is the most common cause of paraneoplastic syndrome. We report a case of EN occurring as a paraneoplastic disease.
A 48-year-old Tunisian woman, a non-smoker with no relevant medical history, presented with painful, erythematous, firm nodules on her legs with ankle swelling. The patient did not report any other symptoms. There were no abnormalities on examination except for moderate fever. An extensive infectious and immunological investigation was negative. Antistreptolysin antibodies were undetectable. Chest radiography showed a focal opacity in the right lung and a CT scan revealed a mass in the lower right pulmonary lobe with hilar and mediastinal lymphadenopathies, a nodule in the right adrenal gland, condensation in the iliac bone and multiple bilateral nodular cerebral expansive processes. Bronchial biopsies revealed a primitive and moderately differentiated adenocarcinoma. No argument for tuberculosis or sarcoidosis was found.
LEARNING POINTS
- Erythema nodosum (EN) can be idiopathic.
- EN has rarely been associated with lung cancer and so the association may be coincidental in our patient.
- The lung cancer was easily identified by chest x-ray in this case and in cases described in the literature.
KEYWORDS
Erythema nodosum, paraneoplastic syndrome, lung cancer
INTRODUCTION
Erythema nodosum (EN) is an inflammatory condition of the subcutaneous fat. It presents as erythematous painful nodules, often on the lower legs. It may be accompanied by systemic symptoms such as fever, malaise and arthralgia. It is a common dermatological condition with many different aetiologies, so appropriate clinical investigations should be carried out.
EN rarely presents as a paraneoplastic syndrome, although it has been reported in patients with haematological malignancies or solid tumours [1]. While lung cancer is the most common cause of paraneoplastic syndrome [1], EN has only been reported twice in association with this cancer [2, 3].
We describe the case of a woman diagnosed with lung adenocarcinoma revealed by EN.
CASE DESCRIPTION
A 48-year-old Tunisian white woman, a non-smoker, without a relevant medical history and no drug intake, presented with a 1-month history of painful, erythematous, firm nodules, mainly on the fronts of her legs with ankle swelling, suggesting EN. The patient reported no other general or specific symptoms. There were no other abnormalities on examination except for moderate fever.
Laboratory tests revealed an inflammatory syndrome: the erythrocyte sedimentation rate (ESR) was 45 mm/hr, C-reactive protein (CRP) was elevated at 108 mg/l (normal range <8 mg/l), polyclonal hypergammaglobulinemia (15.8 g/l) was present, and serum lactate dehydrogenase was elevated at 350 IU/l (normal range: 140–271 IU/l). Calcium and angiotensin-converting enzyme levels were normal. An extensive search for infection (including a tuberculin skin test) was negative. An immunological panel, including anti-streptolysin antibodies, was also negative.
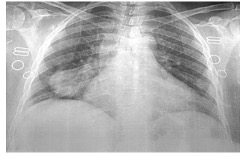
Chest radiography showed a focal, nodular, well-limited para-cardiac opacity in the right lung field (Fig. 1).
Figure 1. Chest radiography showing a mass in the inferior right lung field
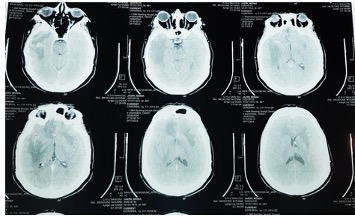
A CT scan revealed a heterogeneous and irregular tissular mass in the lower right pulmonary lobe measuring 61×62×55 cm, with necrotic areas, multiple hilar, mediastinal and abdominal lymphadenopathies, a heterogeneous 13×19 mm nodule in the right adrenal gland, irregular condensation in the right iliac bone, and multiple bilateral nodular cerebral expansive processes (Figs. 2 and 3).
Figure 2. Thoracic computed tomography sections showing the pulmonary tumour Figure 3. Cerebral computed tomography of the brain showing multiple diffuse nodules
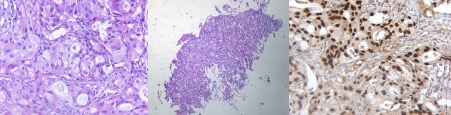
Figure 4 .Histological sections showing primitive and moderately differentiated adenocarcinoma with positive nuclear TTF1 and cytoplasmic CK7 marking
DISCUSSION
Lung cancer is the leading cause of cancer deaths worldwide. In the last few years, it has become more common and severe in women, likely due to cultural and behavioural changes, especially increased smoking. In 2015, the World Health Organization (WHO) noted the frequency of adenocarcinoma compared with squamous cell and small-cell carcinoma, had risen to 50% of all types of lung cancer [4].
Lung cancer is the most common cause of paraneoplastic syndrome, which can occur at any stage of the cancer, precede it by several months or even reveal it. Small-cell lung carcinoma is more frequently associated with paraneoplastic syndromes than adenocarcinoma[5]. These syndromes can be triggered by hormones, peptides, mediators and antibodies secreted by the tumour, but the aetiology remains unclear in many cases. The blood, nervous system, endocrine glands, bones and skin can be affected. Associated skin diseases include woolly hypertrichosis, erythema gyratum repens, acrokeratosis (Bazex syndrome), dermatomyositis, and Sweet syndrome, which are all rare in lung cancer.
EN is the most common clinical form of acute nodular hypodermatitis. The most frequent causes include infections, drugs, pregnancy and systemic diseases such as sarcoidosis and enteropathies. However, no obvious aetiology is found in approximately 50% of cases.
We have described a case of EN revealing metastatic adenocarcinoma in an asymptomatic and non-smoking middle-aged woman. Paraneoplastic EN is rare and the few reported cases were associated with lymphoma, leukaemia, and digestive, gynaecological and endocrine gland malignancies [1]. This association is considered to be a marker of poor prognosis. To our knowledge, only one case of recurrent EN associated with non-small-cell carcinoma has been reported [2].
No particular characteristics of the skin lesions have been noted in cases of paraneoplastic EN except for possible recurrence and resistance to conventional treatment. A systematic search for a malignant cause should be conducted in cases of paraneoplastic EN for early diagnosis and better prognosis. Regression of EN following anti-cancer therapy is a good causal link.
CONCLUSION
Paraneoplastic EN is rare and has not previously been reported in association with lung adenocarcinoma. A search for a solid neoplasm should be conducted in cases of EN.