ABSTRACT
Thrombus in the aortic trunk is a rare complication. We report the case of a 63-year-old patient with a factor V Leiden mutation in whom an aortic arch thrombus was discovered accidentally. Conservative treatment was initiated with therapeutic anticoagulation with low-molecular-weight heparin leading to complete thrombus lysis after 3 months but associated shortly after anticoagulation initiation with a large splenic and limited renal infarctions.
LEARNING POINTS
- Intra-aortic thrombus is rarely diagnosed on routine CT examination.
- Even a complicated aortic arch thrombus can be successfully treated with conservative anticoagulation.
- Vascular systemic embolisms are possible after therapeutic anticoagulation is started.
KEYWORDS
Aortic thrombus, factor V Leiden, anticoagulation, embolism
CASE DESCRIPTION
A 63-year-old woman was admitted in the emergency department with dyspnoea and cough. Her medical history included pulmonary embolisms related to a heterozygous factor V Leiden mutation. She was not on long-term anticoagulation.
Arterial blood gas analysis on admission showed severe hypoxaemia (PaO2 47 mmHg without oxygen) related to pulmonary infiltrates on chest x-ray treated with antibiotic therapy with a combination of amoxicillin/clavulanate acid and clarithromycin (Fig. 1).
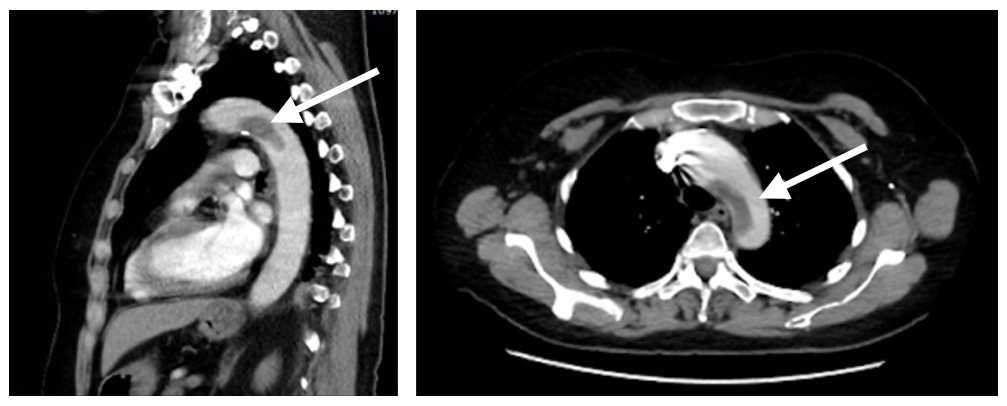
To exclude a new pulmonary embolism secondary to the coagulation disorders associated with factor V mutation, thoracic CT angiography was performed showing no pulmonary embolisms but revealing a large thrombus at the aortic arch junction with the descending aorta, measuring 9 mm in thickness and extending for 5 cm. The most distal part of this thrombus seemed to be detached from the intima-media complex (Fig. 2).
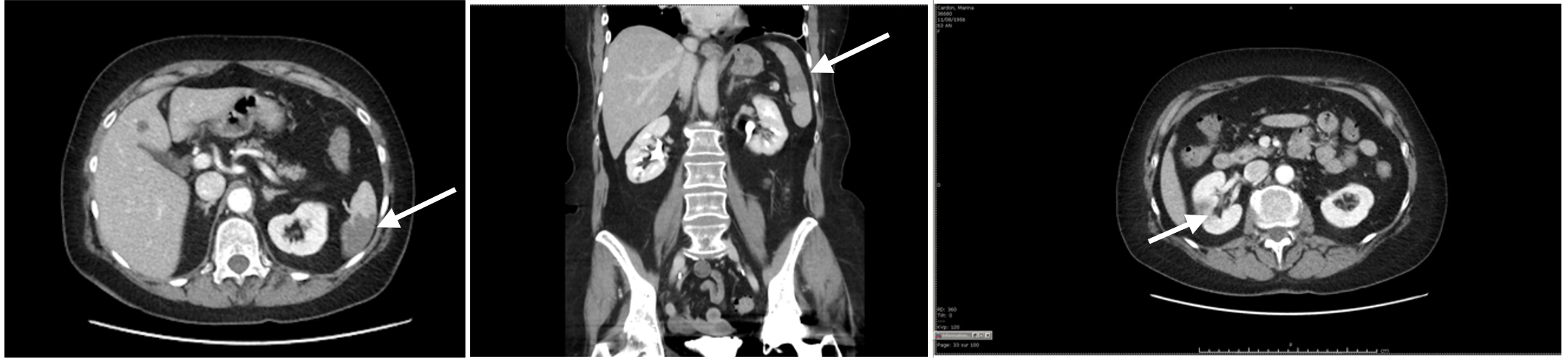
While the patient’s respiratory situation progressively improved 2 days after anticoagulation was started, she developed acute pain in her left upper abdomen. An abdominal CT scan was immediately performed showing a large splenic infarction associated with a possible right renal infarction (Fig. 3). It was decided to continue the conservative therapeutic anticoagulation without surgery. A CT scan performed 3 months later showed complete resolution of the aortic arch thrombus without any new embolic complications or clinical problems.
Figure 1. Chest x-ray on admission showing bibasal infiltrates (arrow)
Figure 2. Thoracic CT angiogram on admission showing a thick thrombus occurring at the junction of the aortic arch and descending thoracic aorta (arrows)
Figure 3. Abdominal CT scan showing a large splenic infarction with a hypodense zone in the middle part of the right kidney related to a renal infarction (arrows)
DISCUSSION
Asymptomatic thrombus in the aortic arch in the absence of underlying atherosclerosis or aortic aneurysm is very rare. Fragmentation is often responsible for acute ischaemic episodes caused by embolisms in various locations like the lower and upper limbs, but also including visceral (renal, splenic, intestinal) and cerebral locations [1, 2].
Aortic thrombi are frequently secondary to coagulation disorders, such as the factor V mutation in our patient, but protein C and S deficiency, homocysteinaemia, elevated factor VIII levels, antithrombin III deficiency, antiphospholipid antibody syndrome, polycythaemia vera, systemic lupus erythematosus, infectious disease, malignancy, trauma and instrumentation can also be responsible for aortic thrombus development [3].
Although most cases of aortic thrombus are diagnosed after embolic events have occurred, some can found incidentally during routine examination, as in our patient: in this case, the embolic complications were probably secondary to the initiation of anticoagulation leading to progressive lysis of the thrombus. Systemic consequences were limited to acute abdominal pain without functional implications related to the splenic and renal embolisms.
The therapeutic approach is still debated and the ideal treatment for such lesions is poorly defined. Treatments should focus on preventing extension of these lesions potentially leading to multiple embolic complications. A variety of approaches are used including thrombolysis, interventional modalities such as thromboaspiration or balloon-catheter thrombectomy and open surgical procedures with thrombectomy, thromboendarterectomy or aortic prosthetic arch replacement [4–6]. Clinical experience remains important in deciding on the therapeutic approach in these uncommon situations, with conservative treatment with anticoagulation remaining another option [7–9].
Most of the published cases reported that aortic thrombi are discovered after an initial thrombotic event leading to the diagnosis. In our case, renal and splenic embolisms probably resulted from the therapeutic anticoagulation for the large aortic arch thrombus diagnosed during a routine CT scan to exclude a new pulmonary embolism in a patient with factor V mutation.
This observation suggests that aortic thrombus could be detected before clinical thrombotic manifestations and confirms that even with a large aortic arch thrombus and embolic systemic complications, a conservative approach with therapeutic anticoagulation can lead to complete resolution of this serious complication of well-known coagulation disorders.