ABSTRACT
Superficial granulomatous pyoderma is a relatively rare variant of pyoderma gangrenosum, characterized by superficial ulceration with a vegetative margin and a clean granulating base. Ulcers in superficial granulomatous pyoderma are typically located on the trunk and may follow minor trauma. It may be misdiagnosed as classic pyoderma gangrenosum, despite having distinct characteristics. Here we report a case of superficial granulomatous pyoderma successfully treated with intravenous immunoglobulin (IVIg).
LEARNING POINTS
- Superficial granulomatous pyoderma is a rare variant of pyoderma gangrenosum.
- Histopathological and clinical characteristics of superficial granulomatous pyoderma are distinct from those of classic pyoderma gangrenosum.
- Superficial granulomatous pyoderma is often slow-growing and is only rarely linked to underlying systemic disease.
- IVIg may be an effective treatment option for superficial granulomatous pyoderma.
KEYWORDS
Superficial granulomatous pyoderma, ulceration, intravenous immunoglobulin
CASE DESCRIPTION
A 68-year-old woman with a history of C1 esterase inhibitor deficiency, Hashimoto’s thyroiditis and hypertension presented with a 3-year history of multiple, slow-growing, superficial ulcers at various sites.
The lesions had originally begun as a single pustule over her right shoulder and eventually progressed to a painful superficial ulcer with a violaceous border and granulating base. Over the following months, several new ulcers developed over the arms, back, abdomen, thighs and buttocks.
Initial treatment with potent topical steroids, hydrocolloid dressings and oral antibiotics was unsuccessful.
Subsequently the patient was admitted to hospital with a productive cough and dyspnoea, during which admission she was given a tapering course of oral prednisolone. This resulted in transient improvement but not complete resolution of the ulcers.
She presented to the Dermatology Department a year later with persistence of the same lesions, which by now had increased in number, enlarged and in areas coalesced to form larger confluent ulcers (Fig. 1).
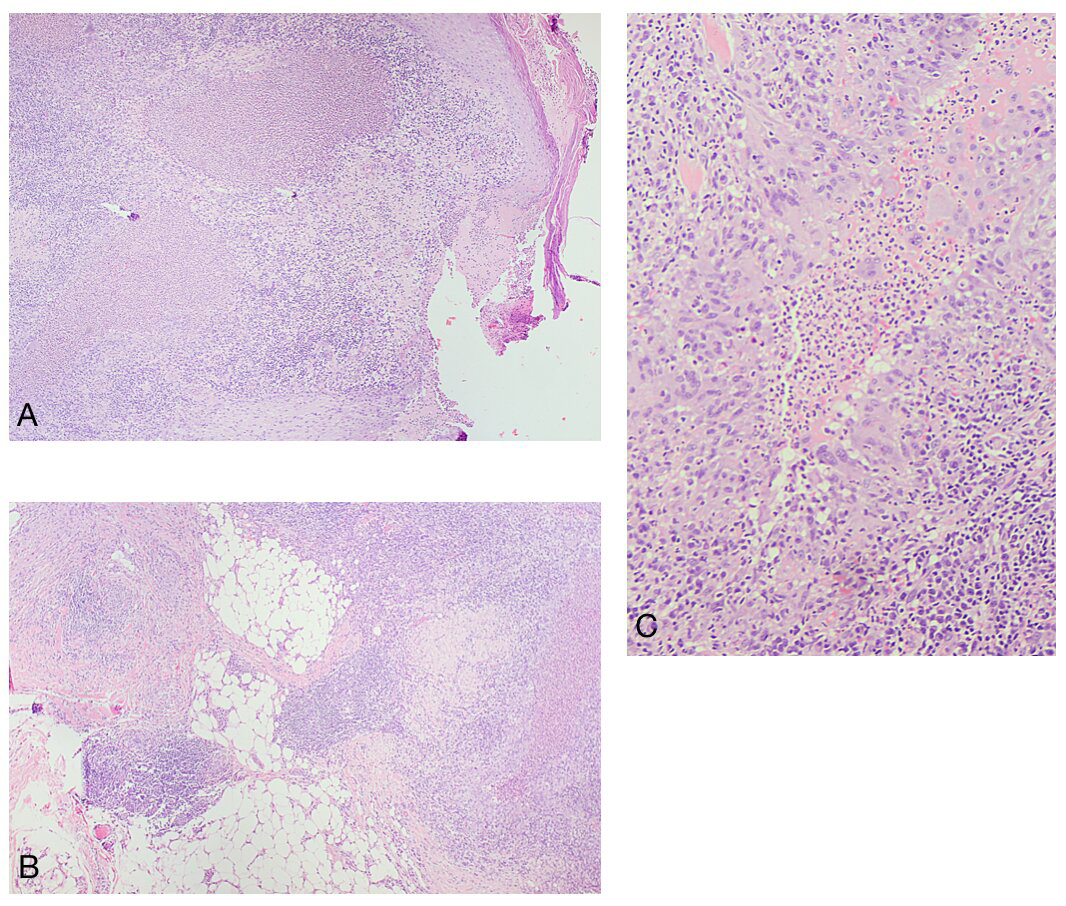
Punch biopsies taken from typical lesions on the right forearm and abdomen showed dermal abscess formation, with sheets of neutrophils surrounded by palisaded epithelioid histiocytes and foreign body-type multinucleated giant cells. There was also extensive dermal fibrosis and a mixed inflammatory cell infiltrate extending into the superficial subcutis (Fig. 2).
Figure 1. Widespread superficial ulceration with a violaceous border and granulating base involving the arms (A, B, C), scapular region (D) and abdomen (E)
Figure 2. Histological analysis showing a dense inflammatory infiltrate with microabscess formation involving the entire dermis (A) and focally extending into the underlying subcu-taneous fat (B) (H&E x40). On higher magnification, a characteristic ‘trilayered’ appear-ance was seen, with a central necrotic neutrophil-rich core, a surrounding histiocytic pali-sade and a peripheral chronic inflammatory infiltrate (C) (H&E x100)
The clinical and histopathological findings at this point were consistent with a diagnosis of superficial granulomatous pyoderma.
Blood investigations including antinuclear, antiglycoprotein, anticardiolipin and antineutrophil cytoplasmic antibodies, extractable nuclear antigen, rheumatoid factor, serum protein electrophoresis and immunoglobulin, complement and angiotensin-converting enzyme levels were all within normal limits. Erythrocyte sedimentation was elevated at 50 mm/hr.
Abdominal and pelvic magnetic resonance imaging, positron emission tomography-computed tomography, colonoscopy and a mammogram, done to exclude possible underlying malignancy, were normal or negative.
The patient was treated with topical tacrolimus ointment and high-dose oral prednisolone followed by a 5-day course of pulsed intravenous methylprednisolone. Despite the cessation of new ulcer formation, the current lesions still persisted. Given the extent of the disease and the patient’s reluctance to receive long-term steroid therapy, together with the known activity of intravenous immunoglobulin (IVIg) in classic pyoderma gangrenosum, a trial of IVIg at a dose of 400 mg/kg/day for 5 consecutive days was given. By the end of the first week of treatment, there were clear signs of improvement, with some reepithelialization and cessation of suppuration.
Over the following 6 months, the patient received 5 similar cycles of IVIg at monthly intervals. All the ulcers healed, with no evidence of recurrence despite tailing down and eventually stopping oral steroids (Fig. 3). The patient was prescribed doxycycline 100 mg daily and topical tacrolimus as maintenance treatment. She remains in remission 2 years after receiving IVIg therapy.
Figure 3. Dramatic improvement of superficial pyodermatous ulcers on the arms (A, B) and abdomen (C) 6 months into treatment with IVIg
DISCUSSION
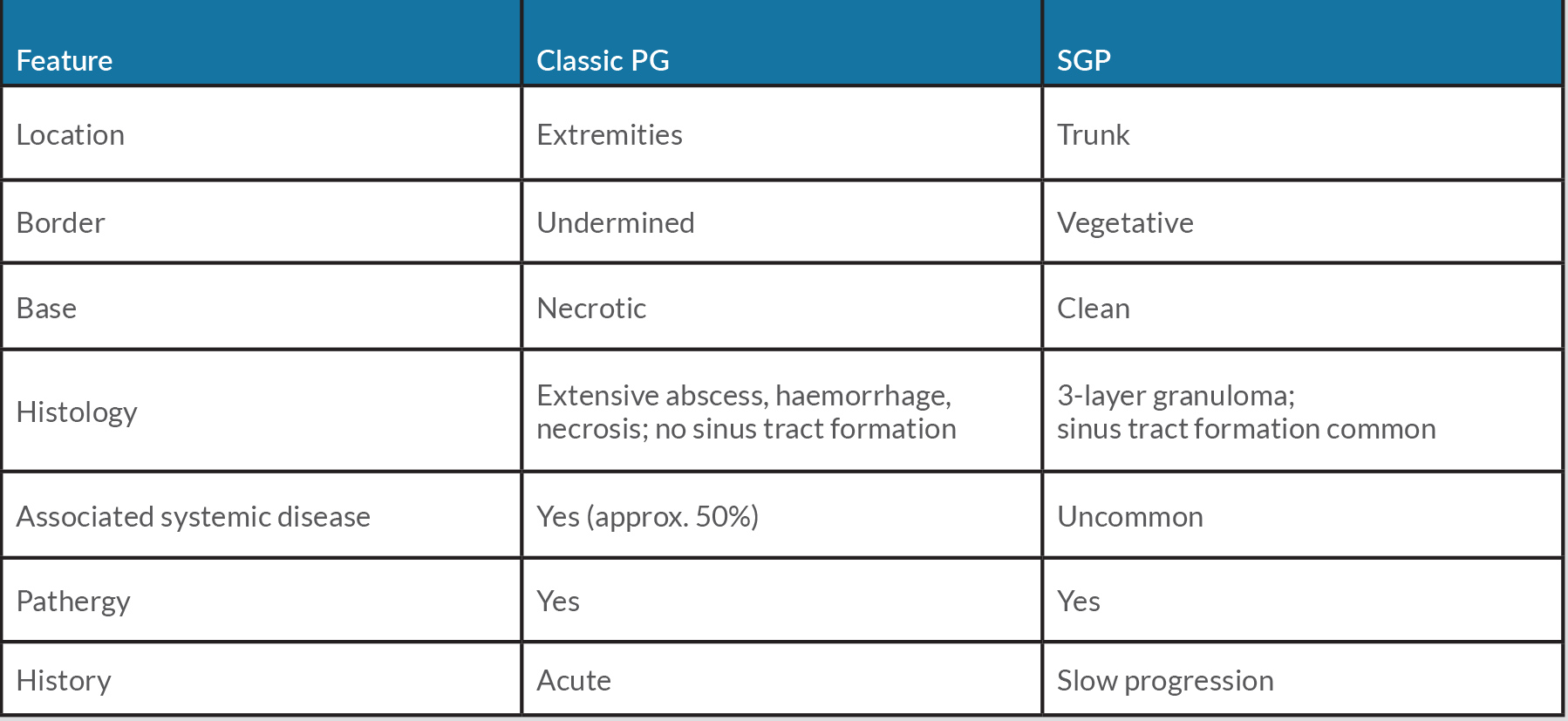
Superficial granulomatous pyoderma, also known as vegetative pyoderma gangrenosum, is a rare variant of pyoderma gangrenosum. Initially described as a separate entity by Winkelmann and Wilson-Jones in 1988, it differs from classic, ulcerative pyoderma gangrenosum in various respects (Table 1). Ulcers in superficial granulomatous pyoderma tend to be more superficial, with a clean base and vegetating borders. There is a predilection for truncal involvement and, unlike pyoderma gangrenosum, superficial granulomatous pyoderma is not commonly associated with underlying systemic disease [1].
Superficial granulomatous pyoderma typically follows an indolent course, often with good response to conservative treatment. This contrasts with the more aggressive behaviour of classic pyoderma gangrenosum [2, 3]. Both conditions, however, demonstrate pathergy and healing with cribriform scarring. While superficial granulomatous pyoderma has been reported to typically manifest as a localized, solitary lesion [1], our case was unusual in that several ulcers developed at different sites over a 3-year period before effective treatment was commenced.
While there are no pathognomonic histopathologic features of superficial granulomatous pyoderma, several typical findings have been defined including the characteristic 3-layered granuloma: an innermost zone composed of necrotic debris and neutrophils, a middle layer of giant cells and histiocytes and an outer layer of plasma cells, eosinophils and dilated blood vessels [2]. In addition, sinus tract formation as well as pseudoepitheliomatous hyperplasia and epidermal acanthosis may be present (Table 1).
Table 1. Comparison of classic pyoderma gangrenosum and superficial granulomatous pyoderma
Systemic corticosteroids are widely regarded as first-line treatment for superficial granulomatous pyoderma, although the condition may respond to more conservative options, including antibacterials such as doxycycline [4], dapsone [5] and sulphonamides [1], topical or injected steroids and tacrolimus ointment [6]. In cases of steroid-resistant disease, or where steroids are contraindicated, other systemic therapies including cyclosporine [7,8] and infliximab [9] have been successfully employed.
IVIg is an antibody-containing blood product that has become an established treatment option for several dermatological indications including classic pyoderma gangrenosum. IVIg is often effective and well tolerated. Common side effects include headaches, fever and myalgias which are often transient and self-limiting. Rarer and potentially fatal adverse effects include anaphylaxis, neutropenia and renal failure. A systematic review of 49 cases of classic pyoderma gangrenosum treated with adjuvant IVIg reported a complete or partial response in 88% of patients [10]. However, to our knowledge, there has only been 1 case of superficial granulomatous pyoderma treated with IVIg reported in the English literature to date [11]. Several potential mechanisms of action of IVIg in halting the inflammatory process in superficial granulomatous pyoderma have been proposed. The most significant of these is the generation of a membrane attack complex, with anti-idiotypic antibody constituents of the IVIg potentially inhibiting autoantibody activity [11].
CONCLUSION
We describe an unusual presentation of superficial granulomatous pyoderma, itself a rare variant of pyoderma gangrenosum. The excellent clinical response to IVIg in our patient suggests that the drug represents a potential therapeutic option for this condition although randomized controlled trials are necessary to confirm efficacy.