ABSTRACT
Pulmonary coccidioidomycosis and pulmonary actinomycosis are unheard of as co-pathogens. Infection with these organisms on their own can mimic lung cancer, thus presenting a diagnostic challenge. We present the case of a 75-year-old woman presenting with haemoptysis with a chest CT chest finding of a lung mass suggestive of lung cancer. A diagnosis of concomitant infection by Coccidioides posadasii/immitis and Actinomyces odontolyticus was made based on culture and histopathology results. The patient was successfully treated with a combination of antifungal and antibacterial therapy. This is the first reported case of co-infection by these two microorganisms.
LEARNING POINTS
- Pulmonary coccidioidomycosis and pulmonary actinomycosis can mimic lung cancer.
- The diagnosis of infection by Coccidioides posadasii/immitis and Actinomyces odontolyticus is best obtained by histopathology and tissue culture.
- Treatment comprises a combination of oral azoles and a beta-lactam antibiotic for a total of 12 months.
KEYWORDS
Actinomyces, actinomycosis, Coccidioides, coccidioidomycosis, co-infection
INTRODUCTION
Pulmonary coccidioidomycosis, also known as Valley fever, is caused by inhaling arthroconidia of Coccidioides species, and occurs in the United States mostly within the endemic regions of California, New Mexico, Arizona and Texas [1]. Pulmonary actinomycosis, on the other hand, is commonly caused by aspiration of oropharyngeal organisms [2]. Pulmonary coccidioidomycosis and actinomycosis can often mimic lung malignancy with respect to clinical presentation and imaging findings [3]. Concomitant infection with these two microorganisms has not previously been reported in the literature. We present the first reported case of concomitant pulmonary actinomycosis and coccidioidomycosis in an immunocompetent individual.
CASE DESCRIPTION
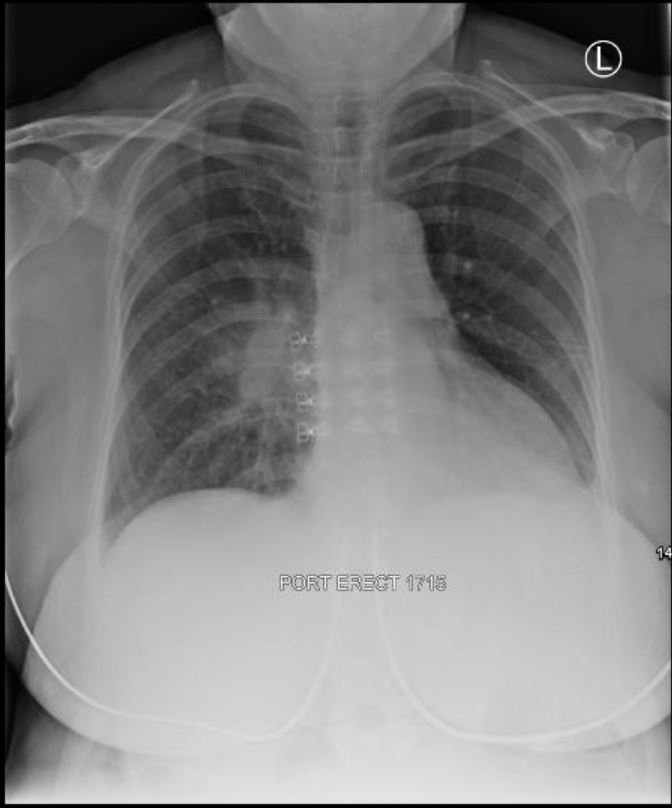
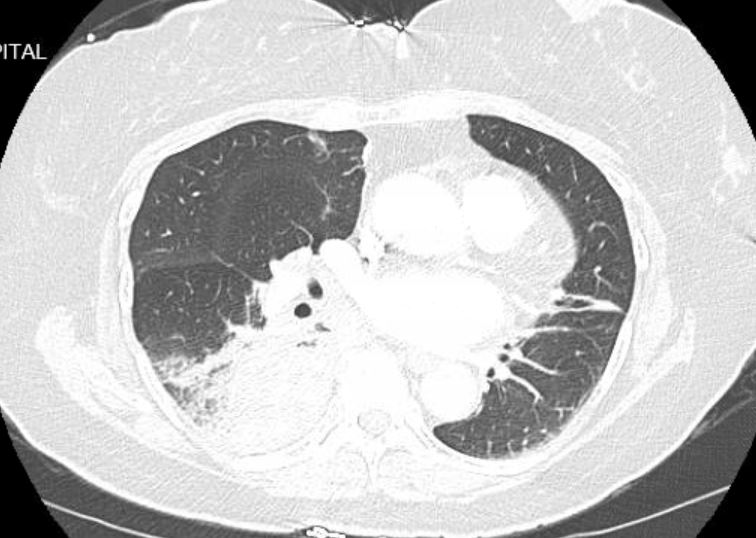
A 75-year-old fourth generation Asian American non-diabetic non-smoker female presented to an emergency department in Arizona with complaints of fever and dry cough. Her past medical history included hyperlipidaemia and atrial fibrillation for which she was taking rivaroxaban. Chest x-ray (CXR) (Fig. 1) showed a prominent right hilar contour and a chest CT (Fig. 2) revealed dense consolidation in the right lower pulmonary lobe (RLL) with some mild hilar and mediastinal adenopathy. She was diagnosed with community-acquired pneumonia and was discharged after treatment with ceftriaxone and azithromycin.
Figure 1. Chest x-ray showing right hilar prominence
Figure 2. CT of the chest showing dense consolidation in the right lower pulmonary lobe with hilar and mediastinal adenopathy
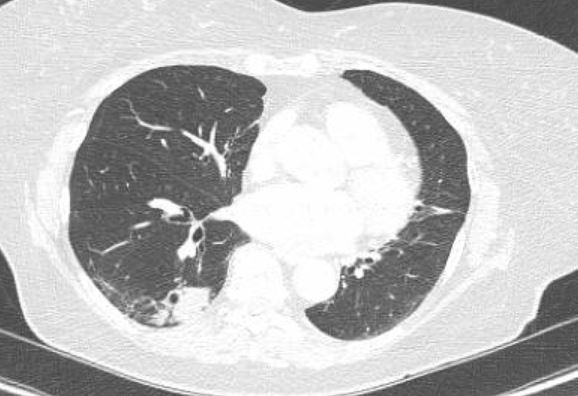
Three months later, the patient returned to the outpatient clinic with persistent symptoms. A follow-up chest CT (Fig. 3) showed a 5 cm RLL heterogenous mass with right hilar and subcarinal lymphadenopathy. These findings were concerning for an unresolved infectious process versus malignancy. The patient underwent outpatient bronchoscopy with biopsy. Results remained inconclusive due to inadequate specimen collection. She then underwent a CT-guided biopsy of the RLL mass which showed necrotizing granulomatous inflammation with silver/fungal staining positive for yeast forms initially identified as that of Blastomyces species. The patient was admitted to hospital when she developed haemoptysis.
She was afebrile and haemodynamically stable. There were no relevant physical exam findings. Laboratory evaluation showed mildly elevated transaminases with ALT of 80 U/l and AST of 72 U/l. The haemoglobin level was normal at 13.1 g/dl and INR was stable at 1.0. Serum fungal antibody testing (using enzyme-linked immunoassay (EIA)) including Aspergillus, Blastomyces, Histoplasma and Coccidioides were all negative. Urine histoplasma antigen and urine blastomyces antigen testing were both negative. CXR showed re-demonstration of the RLL mass with no new focal consolidation. CTA of the chest (Fig. 4) did not show a pulmonary embolism but revealed a dominant RLL mass-like consolidation slightly decreased in size from previous study and a progression in disease pattern with new nodularity in the RLL and right middle lobe (RML). Nodularity in this case was suggestive of a granulomatous disease process such as a chronic incompletely treated fungal infection. Cultures of the specimens obtained by CT-guided biopsy rapidly grew Coccidioides posadasii/immitis and Actinomyces odontolyticus. Repeat Coccidioides antibody testing using complement fixation and immunodiffusion was positive.
Review of the histopathology slides confirmed the yeast form as Coccidioides species and not Blastomyces. A diagnosis of pulmonary coccidioidomycosis with actinomycosis was made and antimicrobial therapy with liposomal amphotericin and oral amoxicillin was started.
During her hospital stay, the patient’s symptoms significantly improved. HIV-1/2 Ag/Ab screen, T and B cell enumeration and di-hydro-rhodamine flow cytometry testing for immunodeficiency were unremarkable. Based on available microbiology data, the patient was discharged on a renally adjusted dose of oral fluconazole and amoxicillin. At the 6-month follow-up visit, she reported complete resolution of her symptoms. A repeat chest CT (Fig. 5) demonstrated improvement in the bulk of the consolidation. Since it was not completely resolved, the antimicrobial therapy was extended for 6 more months for a total course of 12 months.
Figure 3. Chest CT showing a 5 cm right lower pulmonary lobe heterogenous mass
Figure 4. CTA of the chest showing a dominant right lower pulmonary lobe (RLL) consolidation and new nodularity in the RLL and right middle lobe
Figure 5. CT of the chest showing improvement in the consolidation after antimicrobial therapy
DISCUSSION
In endemic regions, pulmonary coccidioidomycosis is the aetiological agent in 17–29% of cases of community-acquired pneumonia. Patients can remain symptomatic for up to 4 months after acquiring the infection. It is acquired by inhaling spores of the soil-dwelling fungus Coccidioides [4]. Pulmonary actinomycosis is most commonly acquired by aspiration of the microorganism from the oropharynx. Less common pathways of acquiring the infection are via inhalation, haematogenous spread and contiguous spread from adjacent tissues. Actinobacillus spp., Streptococcus spp. and Haemophilus spp. are some of the most common co-pathogens encountered in pulmonary actinomycosis [5].
Our electronic literature search in the PubMed and Google Scholar databases using the search terms ‘Actinomyces’ or ‘actinomycosis’ combined with the term ‘Coccidioides’ or ‘coccidioidomycosis’ failed to locate any relevant citations. To our knowledge, ours is the first report of concomitant respiratory infection by C. posadasii/immitis and and A. odontolyticus.
Pulmonary coccidioidomycosis and pulmonary actinomycosis often present as a lung mass or infiltrate and therefore are commonly confused with malignancy based on history and diagnostic imaging findings [3, 6]. Nagaoka et al. [7] reported a case that was initially thought to be metastatic malignancy. After malignancy was ruled out, empirical treatment for coccidioidomycosis was started with no improvement and a final diagnosis of actinomycosis was made based on PCR. In certain situations, the clinical picture in the context of an appropriate epidemiological history may justify empiric treatment of coccidioidomycosis, but if patients fail to improve with empiric therapy, other pathogens or co-infections should be considered. Differentiating such benign infections from malignancy using histopathology and specimen culture in these scenarios becomes all the more important since treatment shifts from surgical resection to more conservative medical management.
Treatment of pulmonary actinomycosis is usually with 2–6 weeks of IV penicillin followed by amoxicillin for 8–12 months [2]. Commonly prescribed therapy for pulmonary coccidioidomycosis includes oral azole antifungals for a duration of 3–6 months. However, when the patient is diagnosed with diffuse pneumonia, treatment with IV amphotericin B for a few weeks followed by a year-long course of oral azole is preferred [1].
Our patient was diagnosed in Illinois but she probably acquired coccidioidomycosis when she lived in Arizona (6 months every year for several years). No risk factors for actinomycosis infection (dental issues or aspiration) were identified for our patient. Initial concern for malignancy on CT chest imaging was the main reason why she underwent biopsy of the lung mass which then led to the correct diagnosis. Co-infection with Coccidioides and Actinomyces spp. is rare, but timely diagnosis and treatment can prevent unnecessary invasive interventions.