ABSTRACT
Paraneoplastic Raynaud’s phenomenon has often been reported in leukaemia, lymphoma and sarcoma. Nevertheless, an association with lung cancer is not frequently reported in the literature even though lung cancer is a common malignancy. We present a case of paraneoplastic Raynaud’s phenomenon as the presenting feature of underlying lung malignancy.
LEARNING POINTS
- Raynaud’s phenomenon can be a presenting feature of lung cancer.
- Evaluation for an underlying malignancy is important if the work-up is negative for autoimmune and vascular aetiology.
KEYWORDS
Raynaud’s phenomenon, lung cancer
CASE DESCRIPTION
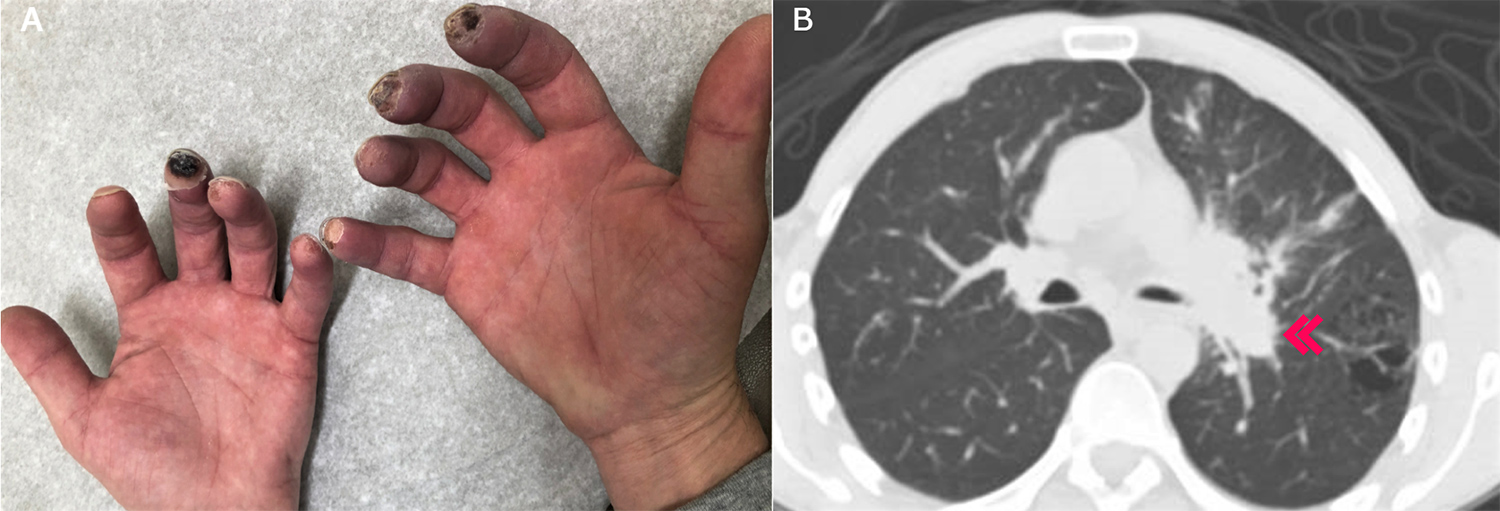
A 51-year-old male construction worker with a 40 pack-year smoking history presented with a complaint of bilateral sudden-onset cyanosis of the fingertips (Fig. 1A) with no precipitating or aggravating factors. He had observed this symptom for 2 weeks in association with cold sensitivity, where his hands would turn white and then red. He complained of sharp pain and swelling in his fingertips and reported a 5-pound weight loss in the past 4–5 months. He denied fever, fatigue, cough, dyspnoea, recent travel, sick contacts, or joint pain. He had no prior history of diabetes or haematological, rheumatological or cardiovascular disorders. He had not seen a physician for many years.
On physical examination, the patient’s vitals were normal. His fingertips were cold and had palpable tenderness and bilateral bluish discoloration. The bilateral radial pulses and dorsalis pedis pulsation were normal and bilateral breath sounds were clear. Cardiovascular and neurological examination was normal.
Work-up, including complete blood count, a comprehensive metabolic panel and thyroid function, was normal. The inflammatory markers erythrocyte sedimentation rate and C-reactive protein were normal. Antinuclear antibody, antineutrophil cytoplasmic antibody and rheumatoid factor were normal. Imaging with computed tomography (CT) angiogram of the bilateral upper extremities showed no occlusions.
A chest x-ray showed increased opacity in the left hilar region. A CT of the chest performed to delineate the opacity better showed a 5.0×4.0 cm left hilar mass lesion (Fig. 1B) with narrowing of the left upper lobe bronchus and multiple mediastinal lymphadenopathies with metastatic lesions in the left iliac bone and spleen. An endobronchial ultrasound-guided biopsy of an interlobar lymph node revealed evidence of metastatic squamous cell carcinoma.
The finger discoloration was presumed to be paraneoplastic Raynaud’s phenomenon in the setting of lung malignancy.
Treatment was started with amlodipine for distal cyanosis. The patient underwent radiation and chemotherapy with carboplatin and paclitaxel, leading to improvement in Raynaud’s phenomenon with a pinker appearance of the fingertips and in the size of the left hilar mass. He was subsequently on durvalumab as maintenance therapy for lung cancer, which he tolerated well, but died 2 months later by massive haemoptysis.
Figure 1. (A) Bilateral cyanosis of the fingertips; (B) CT of the chest showing a 4.9 cm left hilar mass (red arrow) consistent with malignancy
DISCUSSION
Raynaud’s phenomenon is a common clinical condition, with a reported prevalence of up to 5% in the general population. Paraneoplastic Raynaud’s phenomenon has been reported in sarcoma, lymphoma and leukaemia. Few case reports have been published on lung cancer. Raynaud’s phenomenon is also associated with chemotherapeutic agents such as cisplatin and gemcitabine [1].
The pathophysiology is poorly understood but might be related to vasoconstriction of digital arteries, precapillary arterioles and cutaneous arteriovenous shunts. Secondary Raynaud’s phenomenon in the absence of autoimmune or vascular aetiology should prompt investigations for an underlying malignancy. Raynaud’s phenomenon can develop during any phase of cancer and also during treatment [2, 3].
The mainstay of treatment remains calcium channel blockers (e.g., nifedipine), losartan, fluoxetine and captopril. Prazosin has been tried successfully, and iloprost has been described as beneficial for paraneoplastic Raynaud’s phenomenon. Cervicothoracic sympathectomy or localized digital sympathectomy have also been tried for paraneoplastic Raynaud’s phenomenon [1, 2].
Similar cases in the literature include a 54-year-old man with Raynaud’s phenomenon and right lung adenocarcinoma, whose symptoms improved after chemotherapy [3], and a 62-year-old man who sought attention for severe Raynaud’s phenomenon and was found to have non-small cell lung cancer, whose symptoms also resolved after chemotherapy [4].
Wilmalaratna et al. reported the case of a 69-year-old man who had Raynaud’s phenomenon with primary adenocarcinoma of the apex of the left lung [5]. Kopterides et al. described a 65-year-old woman with stage IIIB lung adenocarcinoma diagnosed 6 months earlier who developed Raynaud’s phenomenon, had to undergo amputation of her fingers for gangrene, and later died of respiratory failure [6].
Recently, another similar case has been reported in an 85-year-old man who had paraneoplastic acral vascular syndrome in the setting of recurrent non-small cell lung adenocarcinoma, whose symptoms progressed despite treatment with intravenous iloprost, and who eventually died after 1 month [7].