ABSTRACT
Tracheal tears are an uncommon phenomenon that can occur due to infection, blunt or penetrating trauma or iatrogenic causes secondary to endotracheal intubation or procedures such as bronchoscopy. Post-intubation tracheal laceration is a very rare yet serious complication with high morbidity and mortality rates. Here, we report the case of a 53-year-old woman with a medical history of hypertension who presented with complaints of facial swelling after undergoing arthroscopic debridement of the coracoacromial ligament as well as partial resection of the acromion for impingement of the right shoulder under general anaesthesia. The patient was found to have extensive pneumomediastinum, subcutaneous emphysema, and a large tracheal tear. We aim to highlight this rare complication of endotracheal intubation, discuss the presenting signs and symptoms, and explore the various management options.
LEARNING POINTS
- Iatrogenic tracheal laceration after intubation is a rare but life-threatening complication.
- Prompt recognition and treatment is required to reduce morbidity and mortality.
KEYWORDS
Tracheal tears, tracheal lacerations, endotracheal intubation
INTRODUCTION
Tracheal tear is a rare phenomenon that can occur due to trauma, infection or iatrogenic causes such as endotracheal intubation or bronchoscopy. The trachea is a windpipe composed of C-shaped cartilaginous rings anteriorly and membranous rings posteriorly, running from the cervical region and terminating at the carina. Key surrounding structures include, but are not limited to, the oesophagus, subclavian vessels, azygos vein, vagus nerve and thyroid gland. The incidence of tracheal injury secondary to endotracheal intubation ranges between 0.05% and 0.37% [1]. While more common in the setting of emergent endotracheal intubation, this complication can also occur in the setting of non-emergent intubation. Although physicians can stratify intubation risk using predictors such as the Mallampati score, complications can still arise from factors such as a large neck circumference, enlarged tonsils and other anatomical defects. With an accuracy of 83%, the Mallampati score is a good indicator of intubation difficulty [2].
Patients with tracheal injury typically present with dyspnoea, cough, haemoptysis, and physical examination findings significant for crepitus under the skin [3]. This is indicative of subcutaneous emphysema, a very common finding in these patients [4].
The approach to management of tracheal tear depends on the aetiology and severity. This can be determined by classifying the tear according to the post-intubation tracheal laceration (PITL) level [5, 6]. Each tear can be classified as PITL I, II, IIIa or IIIb based on the depth of the laceration as well as presentation of mediastinitis. Severe cases require surgical repair; however, conservative management such as endotracheal stenting or fibrin glue can also be a viable option in less severe cases [6, 7, 8]. Long-term sequelae of tracheal tears include scarring and narrowing of the airway as well as increased risk of mediastinitis [3, 4].
CASE DESCRIPTION
A 53-year-old woman with a medical history of hypertension presented to the emergency department (ED) with complaints of facial swelling. The day before presentation, she had undergone arthroscopic debridement of the coracoacromial ligament as well as partial resection of the acromion for impingement of the right shoulder under general anaesthesia. A few hours after the procedure, the patient experienced one or two episodes of non-bloody non-bilious vomiting at home. The patient then noticed swelling of her face and mild shortness of breath for which she decided to come to the ED.
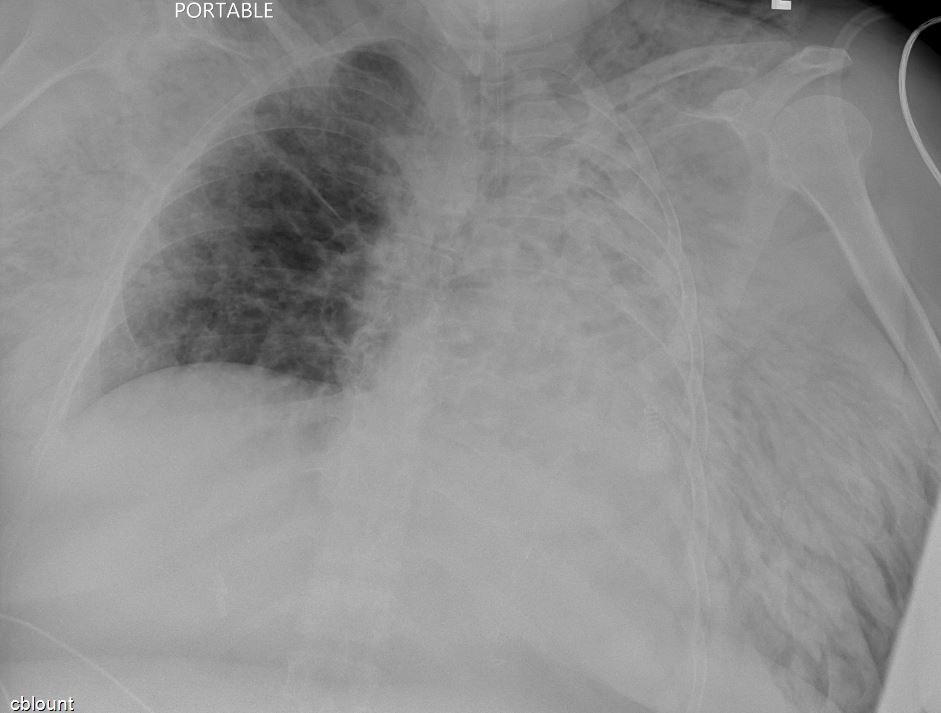
On arrival, the patient was noted to have swelling on the face and neck. She was afebrile, blood pressure was 145/101 mmHg, pulse was 102, respiratory rate was 18, and SpO2 was 87% on room air. On physical examination, extensive crepitation was palpated on the neck, face and chest. Laboratory results showed white blood cells 11.8, haemoglobin 13.8, platelets 231, creatinine 0.74, glucose 171, sodium 134, potassium 4.1 and INR 1.1. Chest x-ray was remarkable for extensive pneumomediastinum and subcutaneous emphysema in the chest, neck and shoulders (Fig. 1).
Figure 1. The chest x-ray was remarkable for extensive pneumomediastinum and subcutaneous emphysema in the chest, neck and shoulders
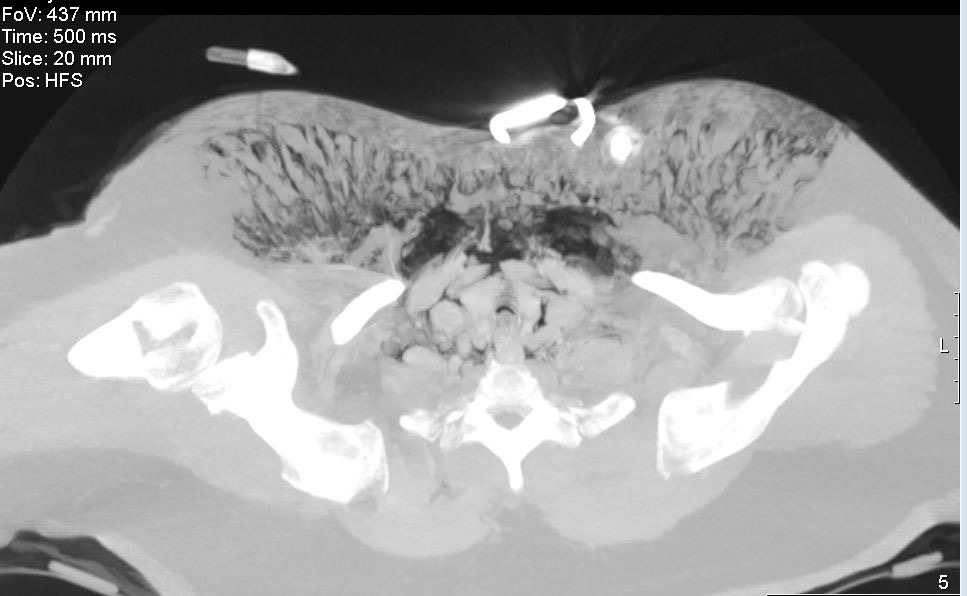
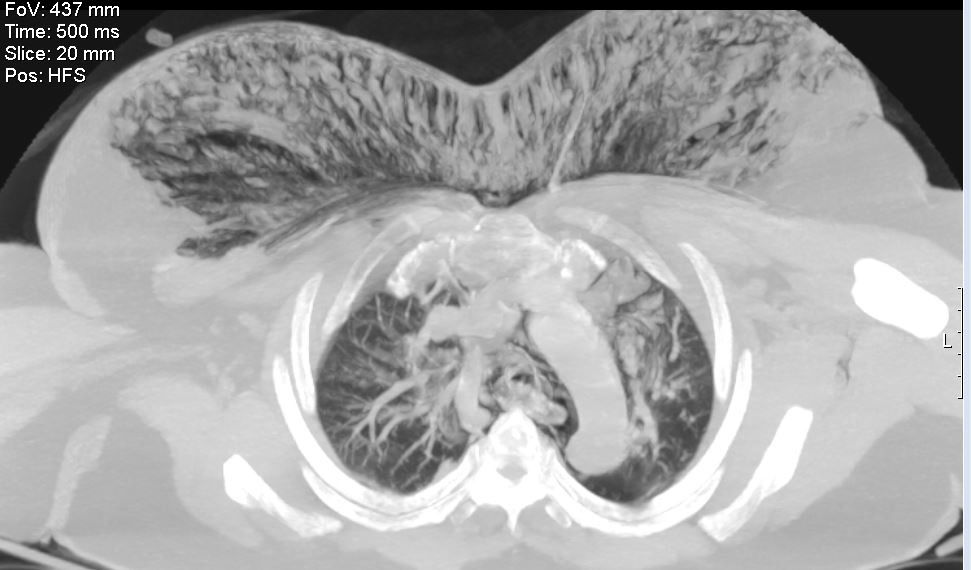
CT of the neck was remarkable for severe and extensive diffuse soft tissue gas throughout the deep and superficial neck and facial compartments including the retropharyngeal and parapharyngeal spaces as well as the masticator space, and diffusely in the neck into the mediastinum and chest wall. CT of the chest showed extensive subcutaneous emphysema and pneumomediastinum, and irregularity of the posterior tracheal wall was noted, suspicious for tracheal perforation (Figs. 2 and 3).
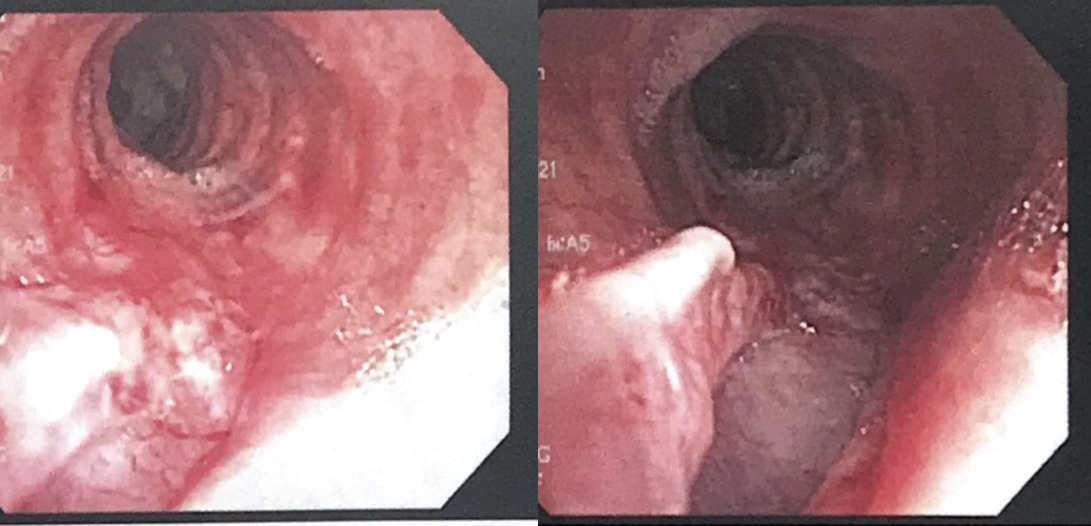
The patient was admitted to the ICU for further management. Gastroenterology was consulted and an oesophagram was performed which showed no oesophageal leak. Pulmonology was consulted and bronchoscopy was done and was remarkable for a large tracheal tear 3 cm from the carina and 3 cm in length in the posterior tracheal wall (Fig. 4). Hence, the patient was intubated with an endotracheal tube placed under direct visualization past the tracheal injury.
The patient was taken to the operating room by cardiothoracic surgery for potential exploration of the trachea and repair, but upon re-evaluation with bronchoscopy, it was found that the tracheal injury seemed to be in the cervical region which can be best approached via the cervical region by ENT. Hence, the patient was transferred to a tertiary care centre for definitive care.
Figure 2. CT of the chest showed extensive subcutaneous emphysema and pneumomediastinum, and irregularity of the posterior tracheal wall was noted, suspicious for tracheal perforationsubcutaneous emphysema in the chest, neck and shoulders
Figure 3. CT of the chest showed extensive subcutaneous emphysema and pneumomediastinum.
Figure 4. Bronchoscopy showed a large tracheal tear, 3 cm from the carina and 3 cm in length, in the posterior tracheal wallpneumomediastinum and subcutaneous emphysema in the chest, neck and shoulders
DISCUSSION
Iatrogenic tracheal rupture after intubation is a rare but life-threatening complication that requires prompt diagnosis and treatment. The prognostic factors are difficult to identify in tracheal rupture as the various causative events are dependent on the individual skills and training of the operator and the anatomy of the patient [9]. In recent years, the reported incidence has varied between 1/20,000 and 1/75,000, as newer devices make intubation easier [10]. The exact cause of tracheal rupture after intubation remains unclear. However, several studies have found multiple causative factors such as repetitive forceful attempts, overinflation of the balloon cuff, incorrect tube size, and improper tube positioning [11]. Anatomical variations are also identified in the literature as significant risk factors for tracheal rupture occurring during surgery, and we could not rule this out in our patient. In any case, tracheal injury or laceration can occur along the path taken by the intubation tube, where damage to the mucosa is very likely, even though the patient has no predisposing factors.
Early signs of tracheal rupture that should prompt immediate work-up in a patient who recently had a procedure and has findings of subcutaneous emphysema, respiratory distress and pneumomediastinum [10]. CT of the chest in our patient showed extensive subcutaneous emphysema, pneumomediastinum, and a posterior tracheal wall irregularity, urging a bronchoscopy work-up to locate the tracheal tear and extent of the damage. Although CT imaging is the first-line investigation, Eliçora et al. have shown that fibreoptic bronchoscopy has higher sensitivity [10]. The combination of both CT and bronchoscopy should be utilized when tracheal rupture is suspected.
There is still some controversy surrounding the use of a conservative or surgical approach for treating tracheal rupture after intubation. Deja et al. [12] found that conservative management was preferred for patients who did not require mechanical ventilation and when their emphysema was only mild and stable during ventilation. Studies recommend that surgery is pursued for patients with posterior tracheal wall perforations greater than 2 cm and mainly depends on how proximal[ the injury is to the carina [14].
However, conservative treatment can still be managed in cases where there was no history of pulmonary or mediastinal surgery, as in our patient who underwent debridement for her right shoulder, and is increasingly becoming the mainstay of therapy. A high concentration of oxygen is helpful for subcutaneous emphysema, and some cases have shown that 2–3 cm blowhole incisions in the supraclavicular or infraclavicular region are helpful for releasing subcutaneous air [14]. Other cases have shown that subcutaneous drains are successful at significantly reducing subcutaneous air and can be one of the methods implemented [14].
CONCLUSION
Although tracheal rupture is not commonly seen after surgery or a procedure in a patient, it is imperative to recognize these risk factors for tracheal rupture after intubation and act accordingly to reduce life-threatening outcomes. We believe that proper equipment and safer intubation steps with experienced tube handling can help minimize the complications associated with post-intubation tracheal tears.