ABSTRACT
Eosinophilic granuloma is a localized, non-invasive form of Langerhans cell histiocytosis. It usually develops in the long bones and is more frequent in children under the age of 10 years. It is very rare in adults.
We present the case of a young woman admitted to hospital for persistent refractory left parietal headache, later revealed to be caused by an eosinophilic granuloma.
LEARNING POINTS
- Eosinophilic granuloma is a localized benign form of Langerhans cell histiocytosis.
- It is essential to exclude the presence of bone lesions in other locations and/or systemic involvement.
- The prognosis is good, with surgical resection, when necessary, being a curative intervention, although sometimes (as in this case) a conservative approach is sufficient.
KEYWORDS
Eosinophilic granuloma, Langerhans cell histiocytosis
CASE DESCRIPTION
An 18-year-old woman presented to the Emergency Department with a left parietal headache of 3 weeks duration and no improvement with over-the-counter analgesics. There was no history of head trauma, but she mentioned the spontaneous appearance of a ‘bump’ on her scalp in the left parietal area. She had no relevant medical history. Her only regular medication was a low-dose combined contraceptive pill.
Upon admission to the hospital, her physical examination, including neurological examination, was unremarkable, except for a tender area on her left parietal scalp, with fluctuation on palpation. The pain was indeed refractory to analgesics and non-steroid anti-inflammatory drugs (NSAIDs), so she was started on opioids, with good response.
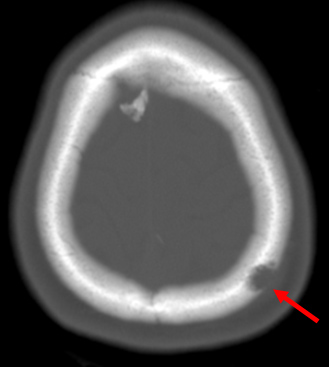
A head computed tomography (CT) scan was performed (Fig. 1). The tender parietal area was revealed to be associated with an 8mm well-defined hypodense lesion in the parietal bone. The bone cortical layer appeared to be involved and there was an epicranial soft tissue component (hence the palpable tender mass on physical examination).
Upon consultation with Neurosurgery, the patient was started on dexamethasone, as the nature of the lesion was uncertain at this point, there appeared to be some local inflammatory oedema, and there was a possibility of intracranial extension, as the internal tabula of the parietal bone did not appear to be intact on the head CT.
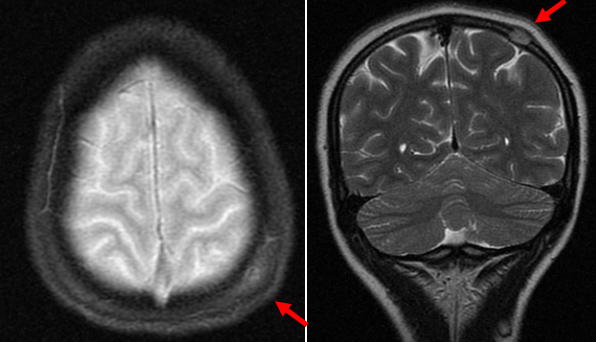
The patient was admitted for clinical surveillance and aetiological study of the parietal bone lesion. There was high suspicion of a malignant bone lesion (primary or metastatic) at this point. A head MRI was performed (Fig. 2) revealing a 10 mm lytic lesion in the parietal bone with‘bulging’of the external tabula of the parietal bone and an epicranial soft tissue extension of the lesion. However, there was no intracranial involvement (as suspected on CT imaging). These findings were highly suspicious of eosinophilic granuloma.
Figure 1. Head CT showing left parietal lytic lesion (red arrow)
Figure 2. Head MRI showing a10 mm lytic lesion in the parietal bone with disruption (‘bulging’) of the external tabula of the parietal bone and an epicranial soft tissue extension of the lesion (red arrows)
The patient underwent extensive imaging and analytical studies for the exclusion of disseminated Langerhans cell histiocytosis. No other bone lesions were found, and there was no evidence of systemic involvement.
Steroid therapy was then tapered and eventually stopped. Opioids were also withdrawn over time with no recurrence of headache. The patient was simultaneously referred to Neurosurgery for surgical resection of the lesion.
However, when she presented at the neurosurgery appointment, she was completely asymptomatic (all medical treatment had already been withdrawn). The parietal lesion was no longer palpable on physical examination. Repeat head CT revealed the same lytic lesion, with very little soft tissue involvement and no evidence of intracranial extension. Considering all this, it was decided not to resect the lesion at this time. The patient has been kept under close follow-up with repeat head CT at 6 months and one year after diagnosis showing no growth in the lesion. She remains asymptomatic. It has been decided that she will be kept under close clinical and radiological surveillance and if/when there is lesion growth and/or new symptoms associated with the granuloma, a surgical resection and biopsy will then be performed.
DISCUSSION
Langerhans cell histiocytosis is a rare disorder with a wide variety of clinical presentations. It is particularly infrequent in adults [1] and the possibility of multi-system involvement poses a particular challenge for physicians.
Historically, the diagnosis of Langerhans cell histiocytosis is histological. However, more recently, advances in magnetic resonance imaging permit the distinction between eosinophilic granulomas and other causes of single osteolytic lesions, namely bone metastasis and osteosarcoma [2].
The prognosis is usually good, as in this case. Frequently, there is need for surgical resection, even of single bone lesions as this one, as they are commonly painful, pose a risk of fracture (in long bones) or may grow in the intracranial space, causing neurological deficits [3]. However, as this patient presented with a small lesion, currently asymptomatic, it was decided a conservative approach would suffice for the time being. If/when there is evidence of lesion growth and/or there is recurrence of symptoms (namely headache or neurological symptoms), a surgical resection will then be performed and it is expected that this procedure will be curative.
There are case reports of eosinophilic granulomas responding to treatment with a local steroid injection [4]. In this case, there was a marked symptomatic improvement after a course of systemic steroid therapy. This was probably due to a decrease in the local soft tissue inflammatory oedema, which was, in itself, causing the presenting symptoms, namely the persistent localized pain.
In spite of the generally good prognosis, the appearance of an eosinophilic granuloma poses a diagnostic challenge for the physician, in particular for internists not accustomed to dealing with paediatric illnesses. It may also be a cause of stress for patients who may doubt the benign nature of the tumour.
It is essential to exclude the presence of bone lesions in other locations and/or invasive forms of Langerhans cell histiocytosis with systemic involvement.