ABSTRACT
Background: Hypothyroid crisis, or myxoedema coma, is a rare condition with high mortality and must be treated promptly. Even though it may be unfavourable, most guidelines only focus on intravenous drug administration due to lack of data on oral treatment.
Methods/Results: The course of oral treatment in two patients admitted in our hospital is described. Patients were treated with levothyroxine 1.3 µg/kg and liothyronine 25 µg twice daily, followed after 1 week with only levothyroxine 1.3 µg/kg daily. Oral treatment was successful in both patients without complications or side-effects.
Conclusions: Oral substitution is an appropriate alternative to intravenous substitution, which has potential disadvantages and is associated with higher mortality.
LEARNING POINTS
- Hypothyroid crisis or myxoedema coma is a rare condition with a high mortality rate, so early diagnosis and prompt treatment are necessary.
- High-dose intravenous treatment is associated with higher mortality, so oral substitution may be an acceptable approach, especially as intravenous medicines are not widely available.
KEYWORDS
Hypothyroid crisis, myxoedema coma, oral treatment
INTRODUCTION
Hypothyroid crisis, or myxoedema coma, is a rare condition with a high mortality rate despite treatment (25–50%). It is usually seen in long-standing and severe hypothyroidism or is provoked by infection or acute illness in poorly treated hypothyroidism [1]. Symptoms of hypothyroid crisis are altered mental state, hypothermia, hypoventilation, hypotension, bradycardia, myxoedema, hair loss, dry skin, reduced renal clearance, hyponatraemia and hypoglycaemia. Treatment consists of thyroid hormone replacement (T3 and T4), supportive care, treatment of potential precipitating disease, and glucocorticoids until adrenal insufficiency is ruled out. When the Dutch guideline was being written [2], it was noticed that fast intravenous correction of hypothyroid crisis was associated with a higher mortality rate. In addition, there are very few data on oral substitution in Caucasians.
CASE DESCRIPTION
We present two patients with hypothyroid crisis, who were managed with oral treatment.
Patient A, a 69-year-old Caucasian woman, presented to the emergency department (ED) with two episodes of brief loss of consciousness without prodromal signs. She was experiencing dizziness, fatigue, an increased need for sleep, a 30 kg weight gain and hair loss over the last few years. She had no other complaints.
She was not currently taking any medication. Her past medical history consisted mainly of chronic kidney disease, psychotic depression and hypothyroidism. She had been treated with levothyroxine in the past.
On arrival, her vital signs were as follows: blood pressure 135/78 mmHg, pulse rate 85 pm, temperature 36.9°C, and peripheral oxygen saturation 96%. Physical examination showed a nearly bald woman with clear signs of myxoedema, such as puffiness of the face and eyes and non-pitting oedema of the extremities. Neurological examination was unremarkable. Laboratory results showed TSH 53.23 mU/l (0.27–4.20), total T3 0.3 nmol/l (1.3–3.1), total T4 5 nmol/l (66–181) and free T4 0.4 pmol/l (12.0–22.0). Physical examination, laboratory results, EKG, chest x-ray, urine sediment and CT angiography ruled out underlying infection and other frequent causes of loss of consciousness. The myxoedema score was 25 [3].
After other causes had been ruled out, the diagnosis of hypothyroid crisis was assumed based on clinical presentation, and the patient was admitted to hospital. Treatment was started with one intravenous dose of levothyroxine (200 µg), liothyronine (10 µg) and hydrocortisone (100 mg). Thereafter, we continued with oral administration of levothyroxine 137 µg once daily and liothyronine 25 µg twice daily. Adrenal insufficiency was ruled out with normal fasting cortisol. While hospitalized, the patient developed paroxysmal atrial fibrillation, which is common during both hypothyroid crisis and its treatment, and was treated accordingly.
During treatment, clinical signs improved markedly, and the patient was discharged after 5 days. At follow-up shortly after admission, it was noted that she had not been taking her medication and she had two more episodes of syncope. Thereafter, she had much better adherence to medication, and levothyroxine monotherapy was continued, resulting in her feeling better, experiencing no fatigue or malaise, regaining normal head hair and losing 16 kg in weight. Laboratory results are shown in Table 1.
Patient B, an 84-year-old Caucasian woman, presented to the ED with lowered mental state (E4M6V1) with syncope beforehand, urine incontinence, apathy and possible left-sided arm paralysis.
Her medical record revealed hypothyroidism, hypertension, polymyalgia rheumatica and epilepsy, for which she was receiving appropriate treatment. She was also treated with 75 µg levothyroxine six times a week but showed poor adherence due to fasting.
On arrival, her vital signs were as follows: blood pressure 184/76 mmHg, pulse rate 50 pm, rectal temperature 33.8°C, and peripheral oxygen saturation 98% with 2 L oxygen. Physical examination demonstrated clear signs of myxoedema.
Laboratory results showed a sodium level of 128 mmol/l (135–145), normal CRP and leucocytes, glucose 5.4, TSH 141.50 mU/l (0.27–4.20) and free T4 4.9 pmol/l (12.0–22.0). A chest x-ray showed signs of cardiomegaly with signs of congestive heart failure and possible pneumonia. CT of the head was unremarkable apart from micro-angiopathy. An EKG showed sinus bradycardia and first-degree AV block, but no signs of acute ischaemia. The myxoedema score was 95 [3].
A diagnosis of ischaemic stroke and hypothyroid crisis with possible pneumonia as the precipitating factor was made. The ischaemia was treated with clopidogrel.
Treatment for hypothyroid crisis was started with active re-warming, oral levothyroxine 50 µg daily and oral liothyronine 25 µg twice daily. The paralysis completely resolved 1 day after admission and was attributed to hypothyroid crisis.
Early during the course of treatment, the patient’s lowered mental state resolved, and no syncope was observed. Steady normalization of TSH, T3, T4 and free T4 was observed during hospitalization (Table 1). The patient was discharged after an 11-day hospital stay and remained in good health for 6 months when she died from sepsis.
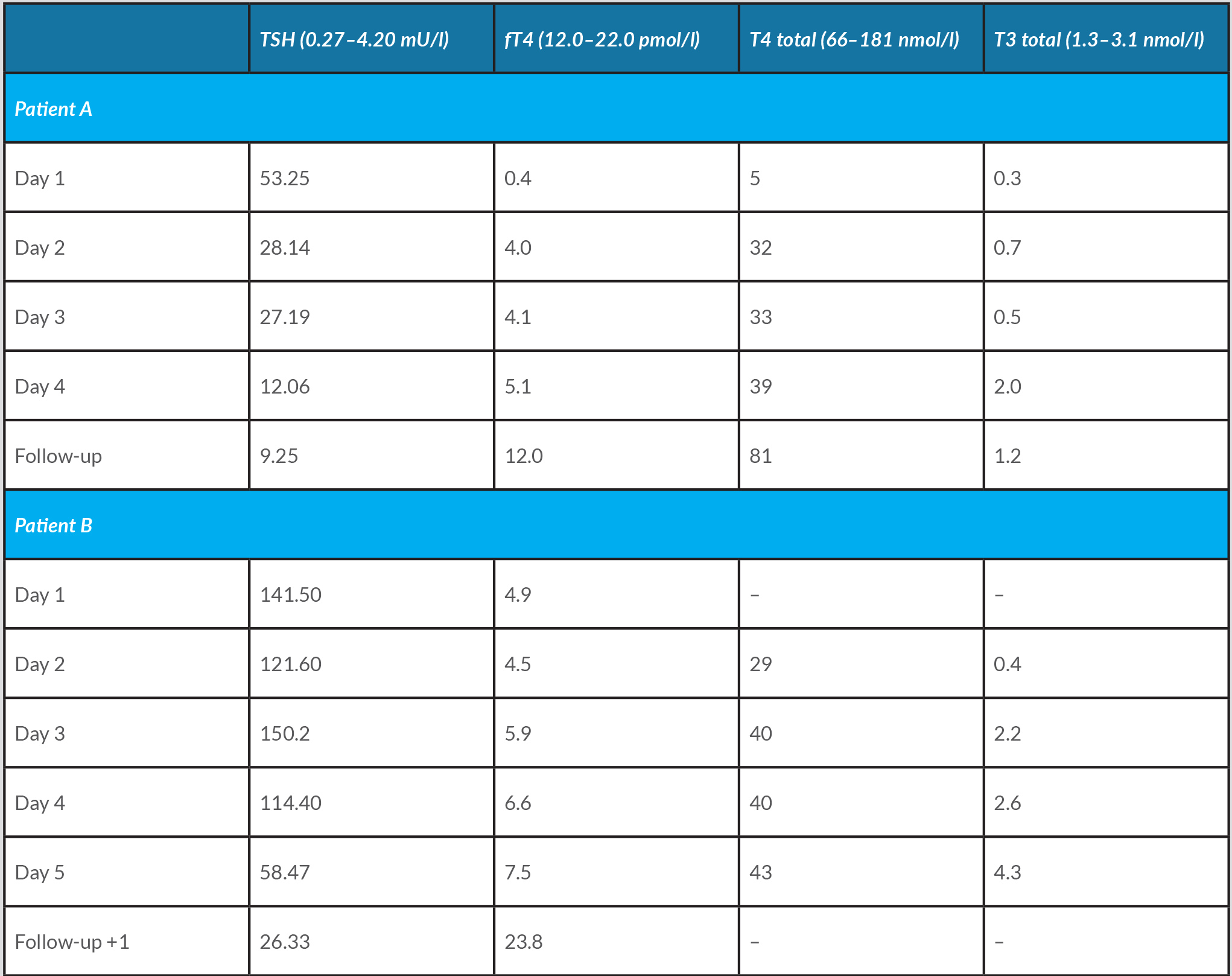
The evolution of thyroid laboratory tests for both patients during admission and follow-up is shown in Table 1.
Table 1.Evolution of thyroid laboratory tests for both patients during admission and follow-up/p>
DISCUSSION
By our knowledge, this is the first case report showing that oral treatment, with both T4 and T3, of hypothyroid crisis is possible in Caucasian patients [4]. Recent publications have demonstrated that oral treatment is possible in Asian patients with oral levothyroxine alone [5, 6]. European guidelines recommend intravenous substitution therapy because of assumed reduced intestinal absorption with oral treatment[7]. Intravenous substitution is an effective and accepted treatment for hypothyroid crisis, but intravenous levothyroxine and liothyronine are expensive, difficult to acquire and associated with cardiovascular complications [8]. Our experience suggests that oral substitution is possible in Caucasian patients with hypothyroid crisis. In the first patient, we decided to start with an intravenous dose, and after consent, continued with oral medication. In the second patient, consent was available immediately and we decided to start with oral treatment. The clinical conditions and laboratory results of both patients were closely monitored during treatment. The strategy for oral treatment was to start with a combination of long-acting T4 and fast-acting T3 and to continue after approximately 1 week with T4 replacement only. We chose this regimen as it was expected that T4 would take longer to achieve steady state and rapid administration of T3 is one of the cornerstones of treatment of hypothyroid crisis. The patients were treated with levothyroxine 1.3–1.6 µg/kg and liothyronine 25 µg twice daily and after 1 week continued with only levothyroxine 1.3–1.6 µg/kg daily.
CONCLUSION
Hypothyroid crisis is a rare and fatal condition that requires immediate treatment. Management consists of supportive therapy, treatment of precipitating disease and, very importantly, thyroid hormone substitution. Guidelines recommend intravenous substitution despite the potential disadvantages, because more data are available on intravenous treatment. Our and other [4–6] cases show that oral substitution is an appropriate alternative.