ABSTRACT
Acute copper toxicity is uncommon in Western countries and is often the result of accidental consumption or a suicide attempt. We report the case of a 65-year-old man presenting to the accident and emergency department after a suicide attempt with ingestion of Bordeaux mixture, ibuprofen, acetaminophen and bleach. Primary evaluation showed caustic oesophagitis, toxic hepatitis and acute renal injury, which were treated with supportive care. During admission, he developed a non-immune haemolytic anaemia associated with high levels of copper in urine and blood. Chelation treatment with penicillamine was started and evolution was favourable after 1 month of treatment. Copper poisoning can be lethal. Prompt diagnosis and treatment are key for a favourable prognosis.
LEARNING POINTS
- Acute copper intoxication is rare and early clinical suspicion and diagnosis are essential to reduce mortality.
- The diagnosis of copper poisoning should be based on clinical presentation and measurement of urine and blood copper levels in addition to serum ceruloplasmin levels.
- Treatment includes reduction of absorption, supportive measures, management of complications and chelation therapy.
KEYWORDS
Copper poisoning, non-immune haemolytic anaemia, toxicology
CASE DESCRIPTION
A 65-year-old man presented to the emergency room after voluntary acute intoxication with Bordeaux mixture, 4 g ibuprofen, 8 g acetaminophen and 125 ml bleach. In the last 3 months, the patient had developed dyspnoea, fatigue and weight loss (13% of usual body weight over 3 months). He was under medical investigation for suspected lung cancer. At presentation he had nausea, blue-green vomiting and abdominal pain. He was haemodynamically stable and the physical examination was normal. Arterial blood gas analysis showed a mixed acid-base disorder (pH 7.21, paCO2 52 mmHg, paO2 68 mmHg, HCO3- 21 mEq/l, anion gap 20.3, lactate 4.06 mmol/l) with normal methemoglobinemia. Blood tests showed iron deficiency anaemia (Hb 11 g/dl, MCV 71 fl, ferritin 12 ng/ml, transferrin saturation 7%) associated with acute renal injury (creatinine 1.58 mg/dl, urea 39.2 mg/dl). Acetaminophen levels were below the toxic level in sequential measurements (highest value of 11.93 µg/ml). The first approach included gastric lavage and fluid therapy. Endoscopy confirmed caustic oesophagitis. The patient was kept fasting and pantoprazole perfusion was started.
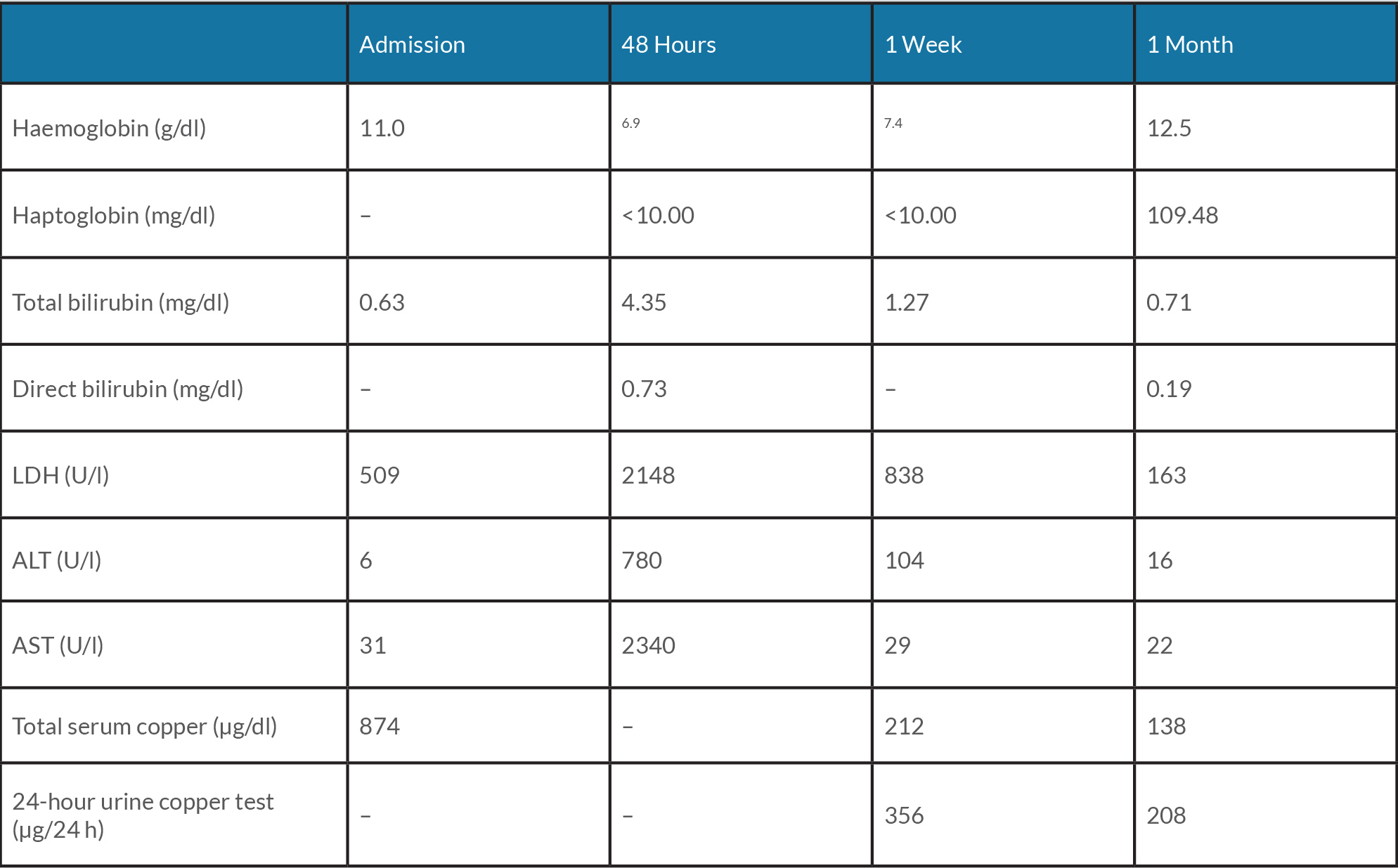
After 48 hours, liver injury was detected with elevation of aminotransferases (AST 2340 U/l, ALT 780 U/l; ratio AST/ALT of 3). The abdominal ultrasound was normal. Jaundice was detected associated with a reduction in haemoglobin levels, without gastrointestinal bleeding. High levels of lactate dehydrogenase, low haptoglobin and increased unconjugated bilirubin (maximum value of 4.5 mg/dl) confirmed haemolysis. The direct Coombs test was negative. Total serum copper (874 µg/dl) and 24-hour urine copper test (356 µg/24 h) were high. In this setting, chelation treatment with penicillamine 300 mg four times daily was started. Progressive clinical and analytical improvement was established and after 1 month, no haemolysis was present and haemoglobin levels were normal. The diagnosis of small cell lung carcinoma was confirmed during the admission. The patient attended the outpatient clinic for psychiatric and oncological follow-up, with good engagement.
DISCUSSION
Poisoning is one of the leading causes of admission to the emergency department. Acute copper intoxication is uncommon in Western countries and is often the result of accidental consumption or a suicide attempt. Bordeaux mixture is a copper-based fungicide used throughout the world [1, 2]. Copper is a catalytic co-factor of many human enzymes and serum concentration ranges up to approximately 1.5 mg/l. The primary source is the diet and its bioavailability is 13–33 days. The major route of elimination is biliary excretion. Toxic concentrations occur after the ingestion of as little as 1 g. About 60% of the ingested dose is absorbed in the gastrointestinal tract and attached mostly to ceruloplasmin (95%). Free copper binds to albumin forming its toxic form [2].
Blue-green material in emesis or stool is highly suggestive of copper ingestion and can be the only clue to diagnosis [3, 4]. In this case, it was possible to confirm the drugs ingested, which is important for clinical management.
The most common manifestations of acute copper intoxication are gastrointestinal (80–100%), haematological and renal (40%). Systemic symptoms can also occur: altered mentation, headache, coma and tachycardia. Gastrointestinal manifestations are usually acute and include a metallic taste, nausea, vomiting, epigastric burning and haematemesis [2, 5]. Our patient presented with caustic oesophagitis that resulted from the combined action of the copper sulphate, ibuprofen and bleach. Toxic hepatitis can also occur as a result of centrilobular necrosis. Due to the low blood levels of acetaminophen, copper was assumed to be the main hepatotoxic drug in our case.
Renal dysfunction is usually mild. Copper causes direct damage to the proximal tubules and acute tubular necrosis can also occur due to hypotension and/or haemoglobinuria.
Intravascular haemolysis usually appears 12–24 hours after ingestion. Haematological manifestations result from red cell membrane damage and due to inhibition of the sulfhydryl groups on enzymes, such as glucose-6-phosphatase and glutathione reductase, which protect cells from free radicals. Copper intoxication can also cause methemoglobinemia.
Initial evaluation of a suspected acute intoxication should include measurements of urine and blood copper levels and serum ceruloplasmin levels. Laboratory findings include anaemia, hyperbilirubinemia, fragmented erythrocytes and Heinz bodies formation. Acute proximal renal tubular dysfunction may lead to aminoaciduria, hypercalciuria, phosphaturia, proteinuria, uricosuria and haematuria. Serum hepatic aminotransferase levels peak within 3 days of ingestion and usually resolve in 1 week [5, 6].
The ‘ABCDE approach’ should be the first step in case management. Specific recommendations for copper poisoning are lacking. Gastric lavage is usually unnecessary due to persistent vomiting. There are no data about the efficacy of activated charcoal. Chelating agents such as penicillamine are recommended in severe poisoning, but little pharmacokinetic data exist to guide their use.
Prognosis is poor if the patient is not treated promptly. Acute mortality ranges from 14% to 36% within a few hours of ingestion.
Suicidal behaviour is a global cause of death and disability. Patient management should include not only treatment of the poisoning but also mental health support and follow-up [5–7].