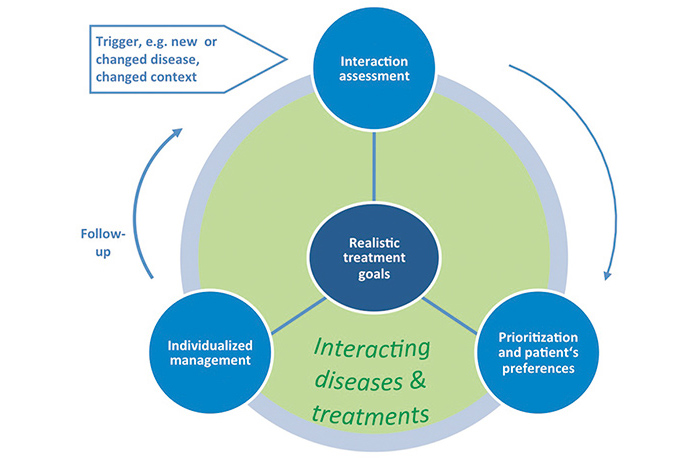
Multimorbidity, the co-occurrence of multiple chronic conditions in an individual, and the frequently associated multimedication is a health issue mostly dealt with in primary care consultations. However, conflicts arising from the application of multiple disease oriented guidelines and the burden of diseases and treatments often make consultations challenging. Situations arise where an individual prioritization is necessary, even when all medications are indicated. This may be the case when interactions of a treatment with one or more existing conditions of the patient (drug-disease interactions) or with co-medications (drug-drug interactions) result in more harm than good. Also, treatment goals may compete with one another and lead to trade-offs in decision making where a balance between two (or more) desirable but incompatible goals has to be achieved. Furthermore, the total treatment burden may be inacceptable to a patient or extend the patient's capacity to cope with. Then priorities must be set. The 'Ariadne principles'[1] have been suggested which describe key principles on how to handle multimorbidity in primary care consultations. Central to the process is the sharing of realistic treatment goals by physician and patient. They result from a thorough interaction assessment of conditions and treatments and a prioritization of health problems that takes into account patient preferences. Individualized management realizes the best (available) options of care (e.g. diagnostics and treatment) to achieve the goals. Goal attainment is followed-up in accordance with a re-assessment during planned visits. The occurrence of new or changed conditions, such as an increase in severity, or a changed context of the patient may provoke the (re‑)start of the process (see Figure 1). With these principles, prioritization is not intended as a unidirectional de-intensification of treatment: a thorough assessment of presenting and continuing problems may identify under-treatment, or the need for intensification, and the elucidation of patient's preferences may show that the patient does not perceive multiple drugs as an unbearable burden. Prioritization is a process of assigning priorities to problems or tasks but does not necessarily mean a reduction.