ABSTRACT
Thrombocytopenia may be the initial presentation of sarcoidosis, which is a systemic granulomatous disorder. Various pathophysiological mechanisms have been identified. Immune thrombocytopenia often has a severe presentation but may respond favourably to immunosuppressive therapy. There are no guidelines for the treatment of thrombocytopenia in sarcoidosis. However, in emergency situations with major bleeding, it seems reasonable to apply the current guidelines recommended for immune thrombocytopenia.
The authors report a case of sarcoidosis presenting with severe thrombocytopenia, petechial rash, and nasal and gingival bleeding.
LEARNING POINTS
- The association of thrombocytopenia with sarcoidosis has been well described and fully documented.
- Immune thrombocytopenia in sarcoidosis is usually severe and symptomatic at presentation but generally has a favourable course because of modern therapeutic management.
- Steroids may be administered as first-line treatment for sarcoidosis, but in emergency situations with a severe bleeding risk, it seems reasonable to apply the current guidelines for immune thrombocytopenia, namely methylprednisolone (1 g/day for 2 days) and/or intravenous immunoglobulin (1 g/kg/day for 3 days).
KEYWORDS
Immune thrombocytopenia, immunosuppressive therapy, sarcoidosis
INTRODUCTION
Sarcoidosis is a multisystemic chronic granulomatous disease of unknown cause with a predilection for the lower respiratory tract [1, 2]. Although haematological manifestations such as lymphopenia and anaemia are often detected, thrombocytopenia is a rare extrapulmonary complication (<1%) [3] and has been rarely reported as the initial clinical manifestation of sarcoidosis [4]. A French review of 20 patients with sarcoidosis and thrombocytopenia concluded that immune thrombocytopenia (ITP) could be severe and symptomatic at presentation but usually followed a favourable course without death or severe bleeding because of modern therapeutic management (mainly immunosuppressive therapy) [2].
The authors report a rare case of newly diagnosed sarcoidosis presenting with severe ITP successfully treated with immunosuppressors.
CASE DESCRIPTION
The authors present the case of a 44-year-old non-smoker female patient with previous obesity, non-medicated dyslipidaemia and recurrent left eye blepharitis, with no usual medication, no history of alcohol, drug or tobacco consumption, and no significant familial medical history.
She was evaluated at the local hospital with complaints of non-pruritic and painless generalized petechial rash, haematomas, and mild gingival and nose bleeding for 3 days. She also complained of mild exertion fatigue (mMRC 2) for about 3 months with no report of fever, cough, anorexia, weight loss, abdominal pain, or other type of blood loss. Physical examination detected predominantly inferior bilateral dry crackles on pulmonary auscultation and the previously described skin alterations. No palpable hepatomegaly, splenomegaly or lymphadenopathy was detected. Blood tests showed severe thrombocytopenia (1.0×109/l), an elevated erythrocyte sedimentation rate (30 mm/h) and high levels of serum angiotensin converting enzyme (SACE; 168.3 U/l, normal range: 8–52 U/l). No pathology other than thrombocytopenia was observed in peripheral smear. The proteinogram and serum electrolytes, lactate dehydrogenase, D-dimer levels, renal function, liver and coagulation tests were normal. HIV/HCV/HBV serologies, faecal Helicobacter pylori, interferon gamma release assay and autoimmunity tests for collagen tissue diseases and vasculitis were negative. Urinary analyses were normal. Chest radiography showed hilar and mediastinum enlargement, and bilateral interstitial-alveolar densifications predominantly in the lower halves (Scadding 2) (Fig. 1).
Figure 1. Chest radiography showing hilar and mediastinum enlargement, and bilateral interstitial-alveolar densifications predominantly in the lower halves
Abdominal ultrasound confirmed the absence of organomegaly. Due to the severity of the thrombocytopenia with a high bleeding risk, 1 g/kg intravenous immunoglobulin (IVIG) was immediately given to the patient, followed by prednisolone 1 mg/kg/day, with symptoms and platelet count improvement after 3 days (>100×109/l).
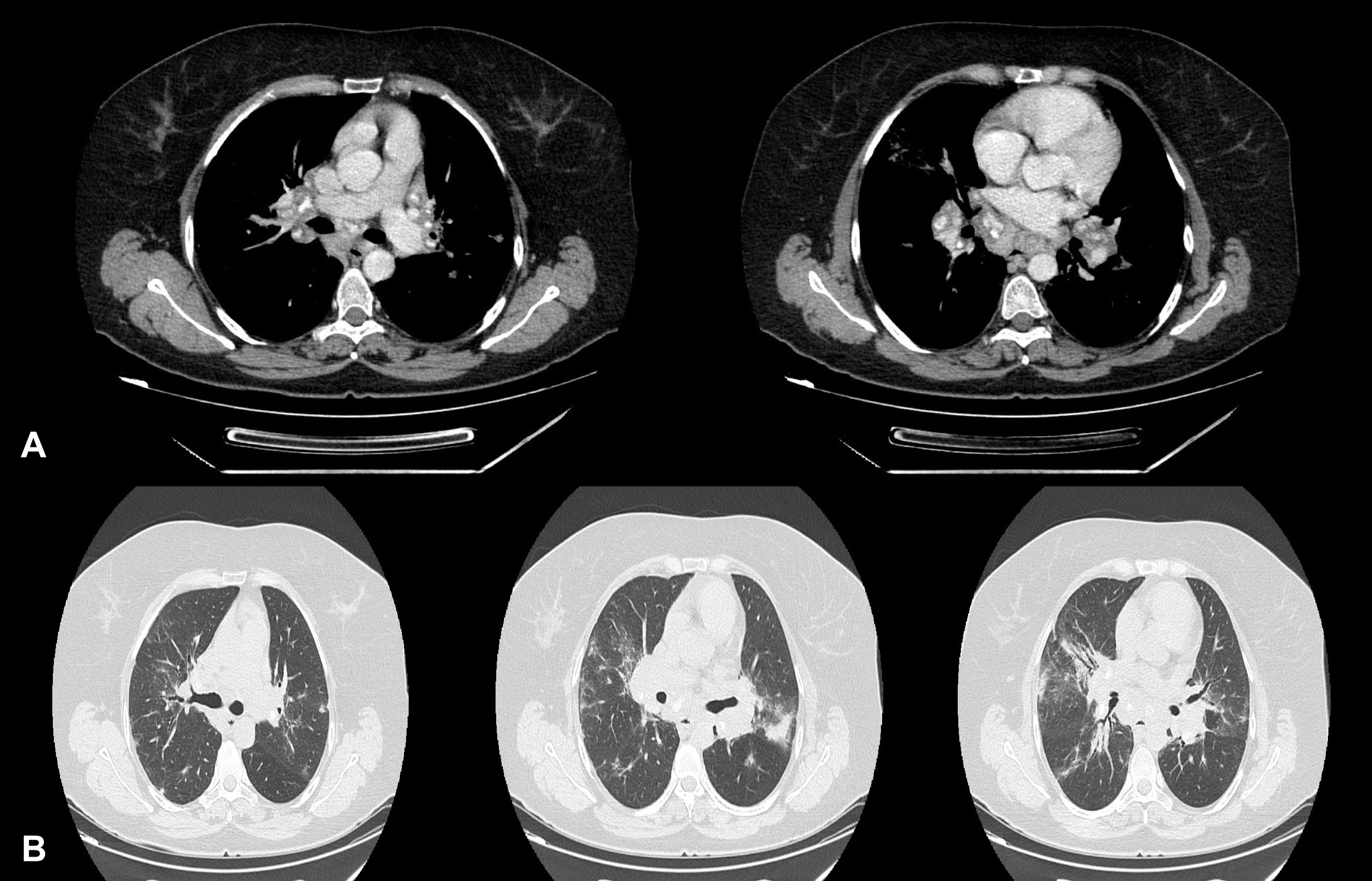
A high-resolution thoracic computed tomography (HRCT) scan was performed, revealing multiple axillar, hilar and mediastinal enlarged lymph nodes, which were symmetrical and bilateral, some with a focal pattern of calcification (Fig. 2A), and generalized parenchymal ground-glass areas with interlobar septal thickening, mainly in the middle and upper lobes, with bronchial wall thickening and air bronchogram (Fig. 2B), with no evident micronodules or other relevant findings. After clinical stability was achieved, flexible bronchoscopy was performed and revealed no relevant endoscopic abnormalities, with bronchoalveolar lavage showing lymphocytic alveolitis (77%) and slight CD4/CD8 ratio elevation (1.88). A transbronchial lung/lymphadenopathy biopsy was inconclusive and a respiratory function test was normal. After steroid withdrawal, the patient underwent lymph node biopsy through mediastinoscopy which showed non-necrotic granulomas without malignant cells, consistent with sarcoidosis.
A final diagnosis of acute sarcoidosis presenting with thrombocytopenia was assumed and the patient started treatment with immunosuppressors, namely methotrexate 10 mg/week and low-dose prednisolone.
Figure 2. Thoracic high-resolution computed tomography showing (A) hilar and mediastinal enlarged lymph nodes, which were bilateral and symmetrical, some with central calcification, and (B) parenchymal ground-glass areas with interlobar septal thickening, mainly in the middle and upper lobes, with bronchial wall thickening and air bronchogram
DISCUSSION
Although rare, the association of thrombocytopenia with sarcoidosis has been fully documented and well described. A study involving 1737 patients with sarcoidosis proved a strong association (OR 8.43) between immune thrombocytopenia and sarcoidosis [5].
The diagnosis of sarcoidosis in our patient was based on the following diagnostic criteria: compatible radiographic presentation and histological evidence of non-caseating granulomas (excluding other granulomatous disease). Also, lymphocytic alveolitis (>15%) with a slightly elevated CD4/CD8 ratio (although <3.5) and an elevated SACE supported the diagnosis. Of note, although the SACE level may be elevated in up to 75% of untreated patients, it lacks sufficient specificity [2]. Moreover, even though our patient started emergency treatment for ITP due to a high bleeding risk before investigations had been completed, clinical stability after steroid withdraw also suggested the diagnosis.
The literature identifies three main mechanisms for thrombocytopenia in sarcoidosis: (i) hypersplenism leading to platelet sequestration and destruction that should be suspected in a patient with splenomegaly and varying degrees of cytopenia (leukopenia, anaemia, thrombocytopenia); (ii) bone marrow granulomatous infiltration with consequent cytopenias; and (iii) autoimmunity with autoantibodies against platelets leading to increased peripheral destruction [2, 3]. Several studies have found that severe thrombocytopenia in sarcoidosis is most probably secondary to an immune process [4–6]. Interestingly, our patient showed no other cytopenia or splenomegaly, her peripheral smear was unremarkable, and there was no identified secondary cause, so primary ITP was assumed. Also, there was a good response to immunosuppression therapy, supporting an immune process causing platelet destruction [3, 5].
There are no guidelines for the treatment of thrombocytopenia in sarcoidosis, but in light of the assumed physiopathological mechanism, steroids may be recommended as first-line treatment. However, in emergency situations with a severe bleeding risk, as in the presented case, it seems reasonable to apply the current guidelines recommended for ITP: methylprednisolone (1 g/day for 2 days) and/or IVIG (1 g/kg/day for 3 days) [3, 4].
Thrombocytopenia and haemorrhage, although quite rare, may be the first presenting signs of sarcoidosis. A high index of suspicion and prompt recognition of clinical features may lead to early diagnosis with good clinical outcomes as the condition may respond to steroids and other immunosuppressive treatment. Well-designed longitudinal natural history studies and long-term follow-up of intervention trials are needed.