ABSTRACT
When stroke patients present with respiratory failure, the first thought that clinicians have is that it is probably related to aspiration pneumonia. However, other causes should be considered, such as intracardiac or intrapulmonary shunts, that could present with paradoxical embolism. Paradoxical embolism is a rare entity defined by the occurrence of a venous thrombotic event associated with a systemic arterial embolism. Frequently, paradoxical embolism presents with platypnoea-orthodeoxia syndrome. Platypnoea-orthodeoxia syndrome is uncommon and is characterized by dyspnoea and hypoxaemia induced by orthostatic position, where symptoms and oxygenation are relieved by recumbency. The authors report a case of a patient who presented with an ischaemic stroke and progression to platypnoea-orthodeoxia syndrome with documentation of simultaneous pulmonary embolism and pulmonary arteriovenous malformations.
LEARNING POINTS
- There are other causes to explain simultaneous presentation of stroke and respiratory failure, which should be kept in mind.
- The association between arterial and venous thrombosis; be aware of paradoxical embolism and search for intracardiac or intrapulmonary shunts.
- Platypnoea-orthodeoxia syndrome is characterized by dyspnoea and hypoxaemia induced by orthostatic position and relieved by recumbency; it is a red flag to think of an intracardiac or intrapulmonary shunt.
KEYWORDS
Ischaemic stroke, pulmonary shunt, paradoxical embolism, platypnoea-orthodeoxia syndrome
CASE DESCRIPTION
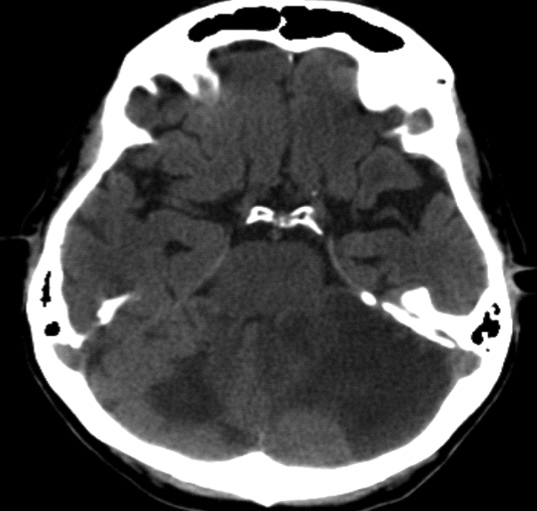
A 74-year-old woman with a previous history of cerebrovascular disease and recurrent episodes of spontaneous epistaxis was admitted to the emergency room due to sudden-onset dizziness and dysarthria with imaging documentation of an extensive bihemispheric cerebellar infarction (Fig. 1). The patient evolved with dyspnoea and hypoxaemia, which worsened upon sitting (platypnoea) and progression to respiratory failure and the need for invasive mechanical ventilation. After endotracheal intubation, the oxygen saturation improved from elevated head (≥30°) to flat-head (0°), and platypnoea-orthodeoxia syndrome (POS) was considered. A transthoracic echocardiogram was performed and did not show an intracardiac shunt. The computed tomography (CT) pulmonary angiogram revealed pulmonary thromboembolism and 3 large pulmonary arteriovenous malformations (PAVMs) in the left pulmonary field (Fig. 2). Endovascular embolization of the PAVMs was performed and there was a progressive increase in oxygen saturation from 85 to 99% at the end of the procedure and the patient was successfully extubated 2 days after the procedure. Besides the PAVMs, the patient also had cerebral arteriovenous malformations, episodes of spontaneous epistaxis and mucocutaneous telangiectasia having been clinically diagnosed with hereditary haemorrhagic telangiectasia (HHT) disorder and the diagnosis was confirmed by detection of a pathogenic sequence variant in endoglin gene (ENG).
Figure 1. Axial cerebral computed tomography showing the bihemispheric cerebellar infarction
Figure 2. Coronal computed tomography pulmonary angiogram revealing multiple PAVMs in the basal left pulmonary segment
DISCUSSION
Aspiration is a frequent sequel of dysphagia and stroke and when the stroke patient presents with respiratory failure, the first thought that clinicians have is that it is probably related to aspiration pneumonia. However, other causes should be considered, from more common to rare ones. A rare cause of simultaneous stroke and respiratory failure is paradoxical embolism (PE). PE should be considered in patients who present with an acute cerebral ischaemic event and respiratory failure. Commonly, PE occurs in the presence of intracardiac or intrapulmonary shunts [1]. In that case, dyspnoea presents such as POS. POS is an uncommon syndrome, first described by Burchell et al. [2] in 1949, characterized by dyspnoea and hypoxaemia induced by orthostatic position and relieved by recumbency [3, 4]. That syndrome occurs in the presence of a functional defect that results in a right-to-left redirection of shunt flow following the upright position. With PAVMs, when the patient assumes a sitting or standing position, gravity increases basal pulmonary blood flow, and in turn, increases blood flow through basal shunts [4]. Since it was first reported, under 200 cases have been reported in the literature [5], although most of the cases described are in the context of intracardiac shunts. The most frequently occurring type of intrapulmonary shunts are PAVMs. PAVMs are abnormal vascular communications directly connecting a pulmonary artery with a pulmonary vein associated with a permanent right-to-left shunt. They are most frequently congenital, usually in the setting of hereditary HHT. The physiological consequences are a permanent right-to-left shunt with multiple potential complications such as brain abscess, seizures and stroke [6]. In rare cases, ischaemic stroke following PE is the initial presentation of PAVMs such as in this case that the authors present. PAVM treatment is indicated in all symptomatic patients and in asymptomatic lesions with arterial diameter >3 mm [6], and the current preferred treatment is percutaneous embolectomy. Early detection of a PE is crucial to improve outcome and clinical suspicion is fundamental to the diagnosis. Clinical presentation with POS and ischaemic stroke should be a "red flag" to warn clinicians they could be facing a PE due to an intracardiac or pulmonary shunt.