ABSTRACT
Infectious sacroiliitis is a rare disease that can occur in conjunction with other osteoarticular infections. Furthermore, it is very unusual for Listeria monocytogenes to be identified in an osteoarticular infection, with spondylodiscitis being the most frequent such infection. We report a case of spondylodiscitis with infectious sacroiliitis due to infection with L. monocytogenes treated successfully with meropenem as salvage therapy.
LEARNING POINTS
- It is very unusual for Listeria monocytogenes to be identified in an osteoarticular infection.
- L. monocytogenes can cause infectious sacroiliitis, which is a rare disease.
- Meropenem has been proposed as salvage therapy and was successful in our case.
KEYWORDS
Spondylodiscitis, sacroiliitis, osteoarticular infection, Listeria monocytogenes
INTRODUCTION
AInfectious spondylodiscitis is defined as infection of the intervertebral disc and adjacent vertebral bodies, and has a prevalence of 3-5 cases per 100 000 population[1, 2]. Infectious sacroiliitis is an inflammation of the sacroiliac joint [3] and is rare, affecting 1–2% of septic arthritis cases. Usually unilateral, it can be accompanied by other osteoarticular infections including spondylodiscitis [4]. Both often occur as a result of haematogenous spread from a distant origin. Medical imaging plays a major role in diagnosis, especially magnetic resonance imaging (MRI[2].
Listeria monocytogenes is a Gram-positive bacillus which causes gastro-intestinal infection and occasionally meningitis and meningoencephalitis, which mostly affect the elderly. It is more common in immunocompromised patients, pregnant women and very old individuals. Contamination usually occurs following consumption of raw dairy products, eggs and meat [5, 6]. It is highly unusual for it to be identified in an osteoarticular infection [7].
We report a case of spondylodiscitis with concomitant infectious sacroiliitis caused by L. monocytogenes.
CASE DESCRIPTION
An 80-year-old woman was admitted to the rehabilitation unit after she fell while on holiday in Algeria. She had vertebral collapse of T12 and L5 and multiple rib fractures. Her medical history included atrial fibrillation, hypertension, diabetes, KDIGO stage IIIa chronic kidney disease and osteopenia. Soon after admission, she developed rigors and fever. The general examination was normal, except for chronic back pain. Blood tests showed an elevated C-reactive protein level of 141 mg/l and blood cultures grew L. monocytogenes after 25 hours of incubation. No gastroenteritis was mentioned by the patient in her medical history, but she confessed to having consumed unpasteurized milk and cheese during her visit to Algeria.
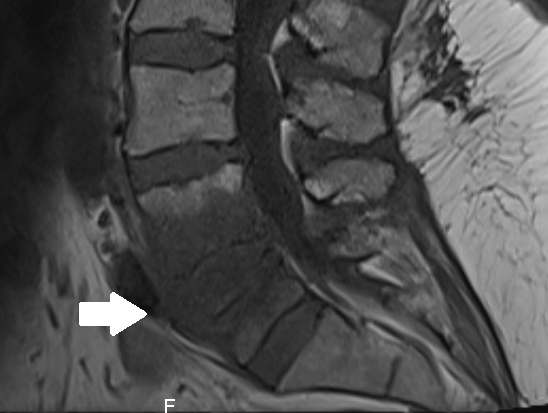
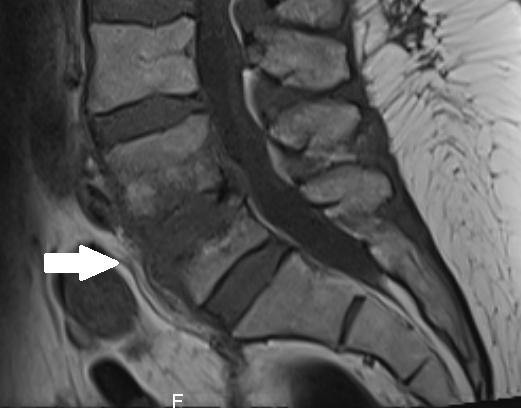
Computed tomography of the abdomen showed L4–L5 spondylodiscitis combined with right sacroiliitis (Figs. 1 and 2). The diagnosis was confirmed with MRI (Fig. 3) and infectious endocarditis was ruled out with transoesophageal echocardiography. Antibiotic therapy with continuous intravenous penicillin and rifampin was first started as bitherapy. Gentamicin was avoided because of the patient’s age and the grade III chronic kidney disease. Rifampin was rapidly switched to cotrimoxazole because of oral intolerance, and treatment was then switched to meropenem on the seventh day, as the patient developed acute kidney injury, leukocytopenia, and recurrent CRP elevation. Meropenem was well tolerated, and the patient’s clinical and biological condition improved. Treatment was prolonged for a further 42 days, MRI at 3-month follow-up showed regression of the lesions (Fig. 4), and no relapse was observed at 1-year follow-up.
Figure 1. CT of the abdomen at the onset of disease showing L4–L5 spondylodiscitis
Figure 2. CT of the abdomen at the onset of disease showing right sacroiliitis
Figure 3. MRI confirming L4–L5 spondylodiscitis at the onset of disease
Figure 4. MRI at 3-month follow-up showing regression of the lesions
DISCUSSION
Listeriosis is a foodborne illness brought about by the consumption of contaminated foods, particularly unpasteurized milk, soft cheeses, vegetables and undercooked meat products. L. monocytogenes mostly causes enteritis with a mild acute fever syndrome, that can sometimes become more severe, mostly in immunocompromised patients. The key risk factors are extreme age, pregnancy, diabetes, cancer, immunosuppressive drugs, autoimmune diseases, HIV, alcoholism and liver cirrhosis [8, 9]. In this case, L. monocytogenes infection was presumably caused by the ingestion of raw dairy products in Algeria.
Pyogenic sacroiliitis is very rare, accounting for less than 2% of infectious arthritis cases. Osteoarticular infection due to L. monocytogenes is unusual with very few cases reported [7, 10–12]. According to Schett et al.[11], joint involvement often occurs in middle-aged patients and usually affects the large joints such as the hip or knee due to haematogenous spread. Spondylodiscitis due to L. monocytogenes has recently been reported [7, 12] but seems to be rare, and to our knowledge, this is the first description of septic sacroiliitis due to listeria.
Regarding medical imaging, MRI is the gold standard to diagnose spondylodiscitis or sacroiliitis, owing to its good sensitivity and specificity[3]. Involvement of soft tissues and the epidural space are best evaluated after contrast injection [12]. In our case, concomitant bacteraemia allowed identification of the causal agent without invasive sampling.
The treatment recommended by guidelines includes amoxicillin or penicillin and gentamicin for at least 6 weeks [2, 7, 13]. Gentamicin should be avoided in case of renal failure or if the patient takes other nephrotoxic drugs [14]. If gentamicin cannot be used, the recommended treatment is a combination of ampicillin plus trimethoprim-sulfamethoxazole (TMP-SMX) [15]. Alternative bitherapy with TMP-SMX and gentamicin is considered in case of suspected immunoglobulin E-mediated penicillin allergy [13]. If neither penicillin nor TMP-SMX can be used, meropenem is an alternative treatment [16]. Meropenem has been proposed as salvage therapy or in intolerance to classic treatment, and was successful in our case.
CONCLUSION
To our knowledge, this is the first published case of spondylodiscitis associated with sacroiliitis due to L. monocytogenes. Listeriosis usually affects pregnant women, and extremely old or immunocompromised patients, and is a rare cause of septic arthritis. The guidelines recommend antibiotic treatment with amoxicillin or penicillin and gentamicin for at least 6 weeks. Meropenem was successful in our case. Medical imaging, especially MRI, and blood cultures played a major role in the diagnosis.