ABSTRACT
We report the case of an 86-year-old female patient with chronic neck pain who presented with an initial misleading clinical picture suggesting an ischaemic stroke. No recent or previous anticoagulation treatment or fall history was reported. The patient developed a paraplegia of the upper limbs needing magnetic resonance imaging which revealed a compressive cervical haematoma. The patient benefitted from cervical laminectomy and evacuation of the cervical haematoma. Motricity in upper extremities was recovered but paresis in the lower extremities persisted 1 week after surgical intervention.LEARNING POINTS
- Insidious spontaneous cervical haematoma can mimic ischaemic stroke.
- Early recognition and treatment of cervical haematoma can improve prognosis.
KEYWORDS
Cervical haematoma, paraparesis, magnetic resonance imaging
CASE DESCRIPTION
An 86-year-old female patient was evaluated at the emergency department at 11 PM for sudden onset of left hemiparesis appearing at 12 midday while she was shopping. Her medical history was relevant for arterial hypertension, type 2 diabetes, cognitive disorders and chronic neck pain secondary to cervicarthrosis. She had received 2 corticosteroid infiltrations a few months earlier. No previous anticoagulation treatment or fall history was reported.
The clinical examination revealed a left hemiparesis not affecting the face. Palpation of the spinous processes from C3 to C6 was painful but the mobility of the spine was normal. Heart sounds were normal and the lungs were clear. An hypothesis of ischaemic vascular stroke was evoked and the patient was sent for a cerebral angiogram of the brain and neck vessels, which did not reveal any abnormality.
The patient did not meet the criteria for thrombolysis, as the time limit was exceeded. Indeed, the eligibility criteria for thrombolysis include a treatment that must be initiated as soon as possible within 4.5 hours of the onset of symptoms. In our case, the delay was 11 hours.
A complete blood assessment including electrolytes, liver, thyroid, renal and coagulation tests was normal. The electrocardiogram showed a sinus rhythm with no abnormalities.
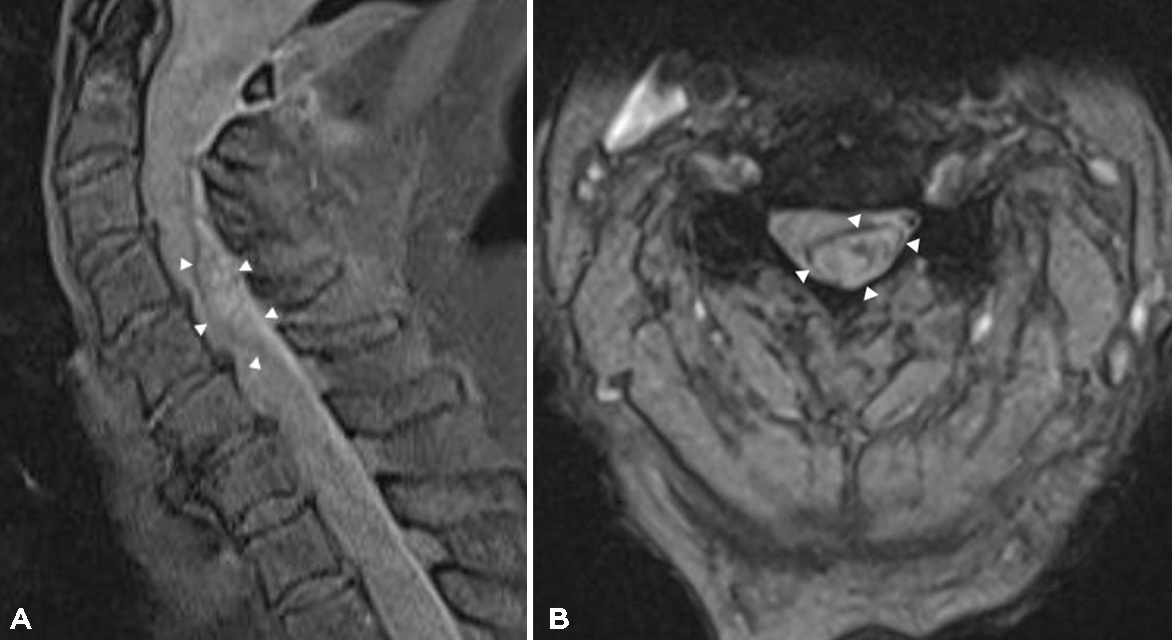
The patient was hospitalized in the observation unit until transfer to the neurovascular unit. The next day, approximately 21 hours after the onset of the initial symptoms, the patient developed paraplegia of the upper extremities progressing to the lower limb, extinction of the osteotendinous reflexes and urinary retention. MRI of the spinal cord was performed and revealed a compressive cervical epidural haematoma extending from C4 to C6 without any argument in favour of an arteriovenous malformation or fistula (Fig. 1). The patient benefitted from cervical laminectomy and evacuation of the haematoma was performed as an emergency. The postoperative course was marked by an improvement in the motor skills of the upper limbs but persistence of paresis in the lower limbs 1 week after surgical intervention.
The patient was then transferred to the rehabilitation department to continue her rehabilitation.
Figure 1. MRI T1W sagittal (A) and axial (B) views show an extensive spontaneous hyperintense epidural haematoma (arrowheads) from C4 to C6. The spinal canal was narrow and the cervical spine was largely deviated without cervical myelopathy
DISCUSSION
Spontaneous spinal epidural haematoma is a rare but serious condition that can be life-threatening and engage functional status. The incidence is estimated at 0.1 cases per 100,000 inhabitants. The cervical location is mostly described in patients between 75 and 90 years of age, while in young patients, the thoracic and lumbar topography is more frequent. The aetiologies are multiple and the main causes are traumatic lesions or complications of spinal medical procedures such as lumbar puncture or epidural anaesthesia, arteriovenous malformations, coagulation disorders, inflammatory or infectious myelitis, spinal tumours of other mention, minor trauma, pregnancy or haemophilia. Anticoagulant therapy can also cause spontaneous haematoma. However, in 40 to 50% of cases no aetiological cause is found and the condition is considered spontaneous [1, 2].
The clinical picture is often atypical, which makes the diagnosis difficult. Patients with spinal haematoma often present with significant pain accompanied by neurological signs. In 95% of cases, neurological involvement occurs at the same time or sometimes after the onset of pain, and may manifest as an isolated sensory syndrome, isolated motor hemiparesis or a sensory-motor stroke.
In the case presented here, the patient had a previous history of chronic neck pain and the initial clinical picture pointed to a stroke. The interrogation was unreliable owing to probable cognitive disorders not previously diagnosed [2, 3]. This contributed to a diagnosis delay of approximately 11 hours, leading to poor functional prognosis after surgery. If the patient had been received within the estimated time for thrombolysis, this procedure could have led to an increase in the haematoma or even death.
Cerebral MRI is the gold standard for diagnosis and therapeutic follow-up. In our case, the hypothesis of a spontaneous haematoma was retained, in view of the absence of fall, previous anticoagulant treatment or other causes. The possibility of a lesion during the 2 previous infiltrations or the cervicarthrosis itself could also have contributed to the haematoma. Cervical haematoma presenting with neurological deficit is considered a neurosurgical emergency and its treatment is based on a cervical laminectomy and decompression of the cord by evacuation of the haematoma. This treatment must be performed within the first 12 hours for a better prognosis, although this time may vary up to 24–48 hours. Some authors suggest that a surgical approach does not offer any benefit if the neurological deficit has existed for more than 36 hours. The prognosis is then conditioned by a rapid diagnosis and management. The functional prognosis depends essentially on the neurological deficit, the extent of the haematoma and especially on the time to surgery [4, 5].
CONCLUSION
Spinal epidural haematoma is a rare but serious pathology that can be life-threatening. With the advent of cervical NMR imaging, diagnosis is easier and earlier. Rapid treatment by surgical decompression allows for better results.