ABSTRACT
The authors present the case of a 79-year-old woman who presented with chronic secretory diarrhoea and severe electrolyte imbalance. A large rectal tubulovillous adenoma was discovered, leading to surgical resection of the tumour with complete resolution of the diarrhoea and electrolyte imbalance. The diagnosis of McKittrick-Wheelock syndrome was made.
We hope this case report will contribute to a greater awareness among health professionals about this clinical condition. A multidisciplinary approach is essential for the best outcome.
LEARNING POINTS
- McKittrick-Wheelock syndrome is an important differential diagnosis in patients presenting with electrolyte abnormalities and secretory diarrhoea.
- A multidisciplinary approach from the beginning is important for a timely diagnosis and better outcome.
- Surgical removal of the hypersecretory villous adenoma is the definitive treatment for McKittrick–Wheelock syndrome and can be life-saving.
KEYWORDS
McKittrick-Wheelock syndrome, electrolyte imbalance, tubulovillous adenoma
CASE DESCRIPTION
A 79-year-old woman with a medical history of dyslipidaemia presented to the emergency department with mucous diarrhoea for the previous 6 months (10 liquid stools daily), without blood or pus. She also reported vomiting, syncope and a 7 kg weight loss (~13% of total body weight). In the preceding 2 weeks, she had been admitted twice to the emergency department (ER) and had been referred to another hospital with the diagnosis of infectious gastroenteritis. Upon admission there was clinical evidence of volume depletion, dry mucous membranes, prolonged capillary refill time and arterial hypotension. No mass was palpable on digital rectal examination. There was abundant discharge of mucus after rectal examination. The remaining physical examination was unremarkable.
Methods and procedures
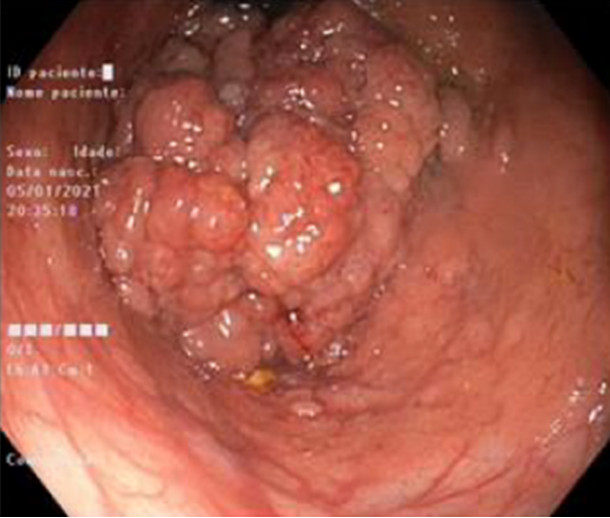
Laboratory findings indicated severe electrolyte imbalance and prerenal acute kidney injury, along with metabolic alkalaemia in relation to volume depletion and hypokalaemia (Table 1, Admission). An HIV test, urine culture, testing for Clostridioides difficile toxins A and B, and bacteriological and parasitological examination of faeces were negative. Anti-Saccharomyces cerevisiae (ASCA) antibodies and an RT-PCR test for SARS-CoV-2 were also negative. Based on these findings an infectious cause was considered less probable.
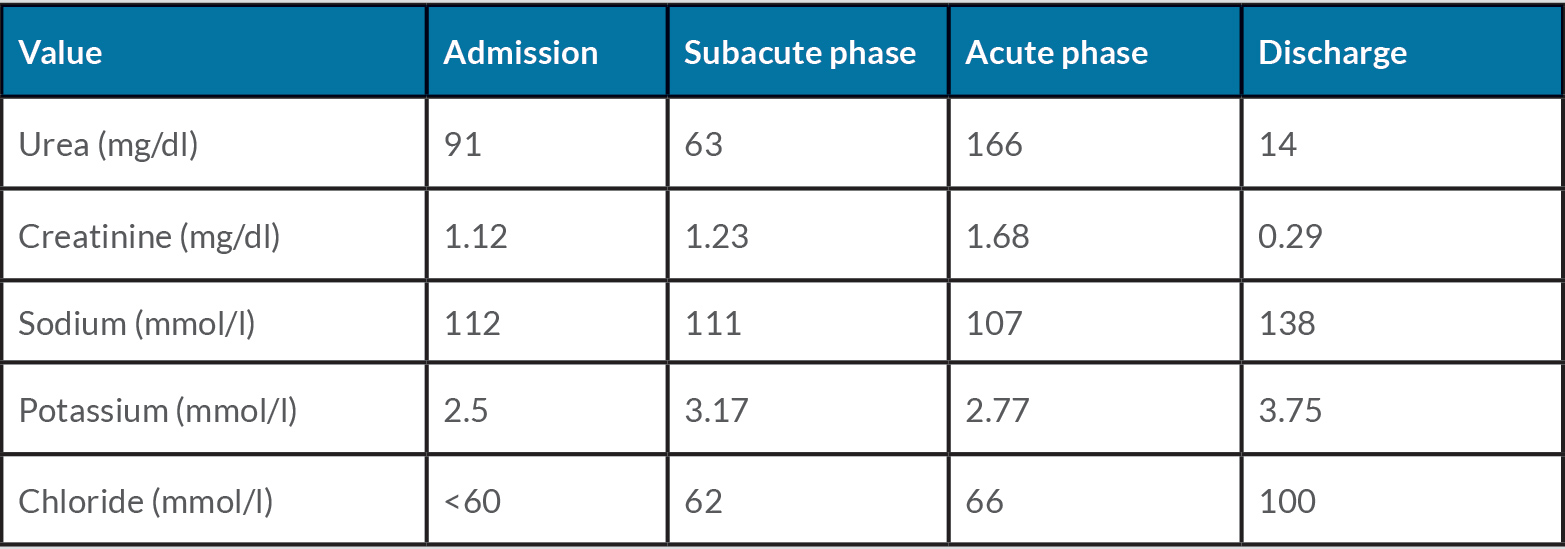
After admission, multiple discharges with large volumes of mucus per rectum were noted (Fig. 1). The amount of mucus was so significant that it was necessary to change diapers several times a day, as well as bed sheets during the night.
The patient improved after fluid and electrolyte replacement with ion, metabolic and renal function normalization. However, after intravenous fluids were stopped, there were two further episodes of orthostatic hypotension with syncope, vomiting and weakness, along with severe fluid and electrolyte depletion and worsening of renal function (Table 1, Subacute phase).
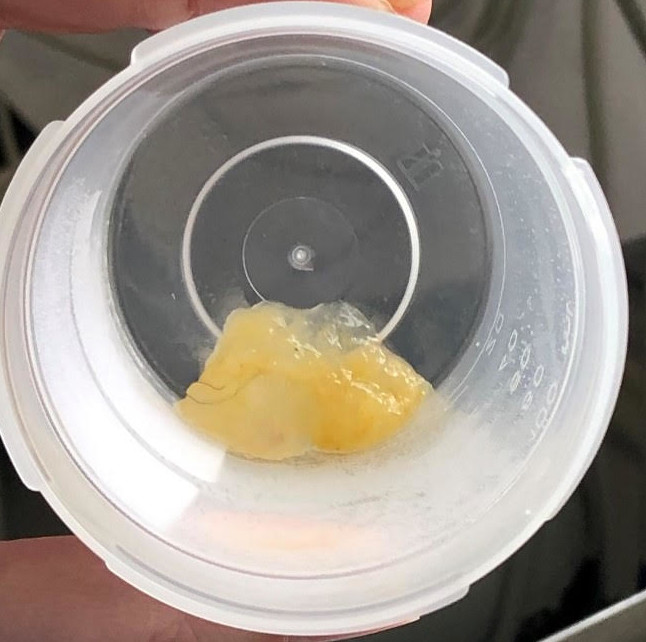
Computed tomography (CT) of the abdomen and pelvis revealed the presence of an endoluminal vegetating lesion that extended from the middle and upper rectum to the last sigmoid loop associated with intestinal dilation, without the presence of lymphadenopathy. These findings were suggestive of a villous tumour (Fig. 2).
Table 1. Laboratory evaluation
Figure 1. Mucus per rectum sample
Figure 2. CT scan (sagittal view) showing a rectal endoluminal vegetating lesion
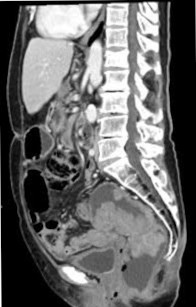
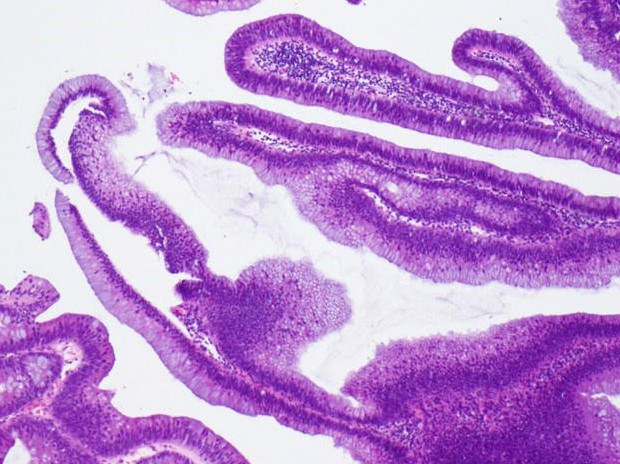
Colonoscopy was performed, which revealed a large villous lesion 17 cm from the anal margin that extended to the first rectal haustra (Fig. 3). Multiple biopsies of the suspect region were performed revealing the presence of a tubulovillous adenoma with low-grade dysplasia (Fig. 4).
For staging, a chest CT scan was performed, showing no evidence of metastatic lesions. It was not possible to perform magnetic resonance imaging (MRI) of the pelvis to better characterize the mass due to patient claustrophobia. Tumour markers CA 19.9 and CEA were negative (<9.00 and 7.20, respectively).
The presence of a hypersecretory tubulovillous adenoma associated with volume depletion and severe electrolyte imbalance was suggestive of McKittrick-Wheelock syndrome.
After intensive therapy with fluids and electrolyte replacement, the patient was started on indomethacin 25 mg every 8 hours, in order to reduce mucus production while waiting for definitive surgery. However, after 8 days of indomethacin treatment there was clinical deterioration with sudden hypovolemic and septic shock. Blood tests at this time showed severe electrolyte depletion and acute kidney injury (Table 1, Acute phase).
After clinical stabilization, the patient was submitted to low anterior resection with end-to-end colorectal anastomosis using a circular stapling device.
Anatomopathological examination of the surgical specimen showed a vegetating lesion 22 cm in length and 8 cm in diameter (Fig. 5). Histological analysis revealed the presence of a tubulovillous adenoma with low-grade dysplasia but no high-grade dysplasia or malignancy. During the postoperative period, the patient was admitted to the intensive care unit due to multiorgan failure.
Figure 3. Colonoscopy image showing a large villous lesion
Figure 4. Tubulovillous adenoma with low-grade dysplasia
Figure 5. Surgical specimen: a large vegetating lesion (22×8 cm)
After tumour resection, there was total remission of diarrhoea with mucus. Serum sodium, potassium and chloride levels returned to normal. The patient gradually recovered and was discharged home partially dependent at the end of her hospital stay (Table 1, Discharge).
Six months after discharge there were no complaints of diarrhoea or mucus passage per rectum. The electrolyte profile was normal. The patient recovered her functional status, resuming normal food ingestion and regaining 6 kg in weight.
DISCUSSION
McKittrick-Wheelock syndrome was first described in 1954, as a rare and benign condition characterized by a large volume of secretory diarrhoea and severe electrolyte depletion secondary to a hypersecretory villous adenoma [1]. The largest and most recent systematic review in 2018 on this subject identified 257 cases described in the literature [2]. However, the current incidence is unknown, and the syndrome may not be as rare as suggested previously, due to the variety of terms used to report the condition. Villous adenomas represent 5% of all colonic adenomas and just 3% of them exhibit secretory activity proportional to their size; they are typically located in the rectosigmoid region [3, 4].
Most patients present with diarrhoea, described as watery or mucous, typically of long duration (median of 24 months) and requiring multiple hospital admissions. The diagnosis is often delayed because of the long duration of symptoms and the first assumption of other diagnoses, culminating in a severe state of volume depletion requiring hospitalization and further investigation.
Electrolyte imbalances are generally universal. Studies have shown that villous adenomas of the rectum demonstrated PGE2 levels three to six times higher than normal [5]. PGE2 serves as a secretagogue and thus induces electrolyte efflux, followed by water drawn out of the rectum.
It is believed that the hypersecretion state might be inhibited by cyclooxygenase inhibitors such as indomethacin. Studies have shown a decrease in faecal content and in the need for electrolyte replacement after administration of indomethacin while the patient waits for surgery, with evidence of decreased levels of prostaglandin in the rectal fluid [6]. Our patient did not respond to indomethacin, in fact she even decompensated. We question its benefit beyond fluid and electrolyte replacement if there is a risk of severe decompensation and risk of life.
Among the cases reviewed in the systematic review mentioned above, more than 50% of patients who had no surgery died [2]. However, most patients achieved complete recovery with aggressive fluid and electrolyte replacement and surgical/endoscopic removal of lesions for full histopathological evaluation. Once the patient is stable, definitive surgery in the index admission is the most favourable long-term management option. Different surgical approaches and intestinal transit reconstructions can be chosen. There is increasing use of minimally invasive techniques, despite the higher recurrence rates and need for multiple procedures [7, 8]. Endoscopic resection is the preferred method, unless it is not possible, and an attempt should be made to reduce tumour volume before proceeding to conventional surgery. A majority of patients received invasive, major and life-changing surgeries involving a high level of morbidity and mortality, such as abdominoperineal resection and anterior resection. These all resulted in full resolution of symptoms and of electrolyte abnormalities [9].
We hope this case report will contribute to greater awareness among health professionals about this clinical condition, which can seriously affect patients and can result in death if not properly diagnosed and corrected in a timely manner. A multidisciplinary approach is essential for the best outcome.