ABSTRACT
Introduction:Carbon monoxide (CO) binds to haemoglobin with a much higher affinity than oxygen, forming carboxyhaemoglobin (COHb), which impairs oxygen transport and utilization. As CO concentrations can easily peak in closed environments, non-fire-related CO poisoning can also occur. However, because CO poisoning is often a nonspecific clinical finding, it can result in a diagnostic error. This report details the misdiagnosis of a 42-year-old male patient with psychiatric disorders.
Case description: The patient presented to the hospital with dizziness, abdominal pain and nausea on multiple occasions. His symptoms were ascribed to his psychiatric conditions. On his fifth visit, we diagnosed the patient with CO poisoning.
Discussion: It is apparent that this patient was misdiagnosed because of his medical history, and standard analysis was overlooked. When patients with psychiatric disorders have nonspecific symptoms, it is important to check for urgent underlying conditions during diagnosis.
LEARNING POINTS
- Patients with psychiatric disorders who present with nonspecific symptoms should be evaluated for underlying conditions, including carbon monoxide poisoning.
- Physicians must make every effort to obtain the accurate medical history of patients with psychiatric disorders.
KEYWORDS
Carbon monoxide poisoning, emergency room, diagnostic error
INTRODUCTION
Carbon monoxide (CO) binds to haemoglobin with a much higher affinity than oxygen, forming carboxyhaemoglobin (COHb), which impairs oxygen transport and utilization. As CO concentrations can easily peak in closed environments, non-fire-related CO poisoning can also occur. However, because CO poisoning is often a nonspecific clinical finding, it can result in a diagnostic error. In addition, patients with psychiatric disorders are generally more prone to misdiagnosis. This report details the misdiagnosis of a 42-year-old male patient with psychiatric disorders.
CASE DESCRIPTION
A 42-year-old man with psychiatric disorders, including panic disorder, anxiety, schizophrenia, attention deficit hyperactivity disorder and epilepsy, presented to our emergency room (ER) 4 times in 1 month because of dizziness, abdominal pain and nausea. At every visit, his vital signs, physical examination findings, laboratory test results and the results of the head, chest and abdominal computed tomography scans were normal. His symptoms spontaneously improved within a few hours of being transferred to the ER. The cause of these symptoms was arbitrarily ascribed to pre-existing psychiatric problems rather than to organic causes. Each time the patient was discharged, it was established that there was little need for further intervention.
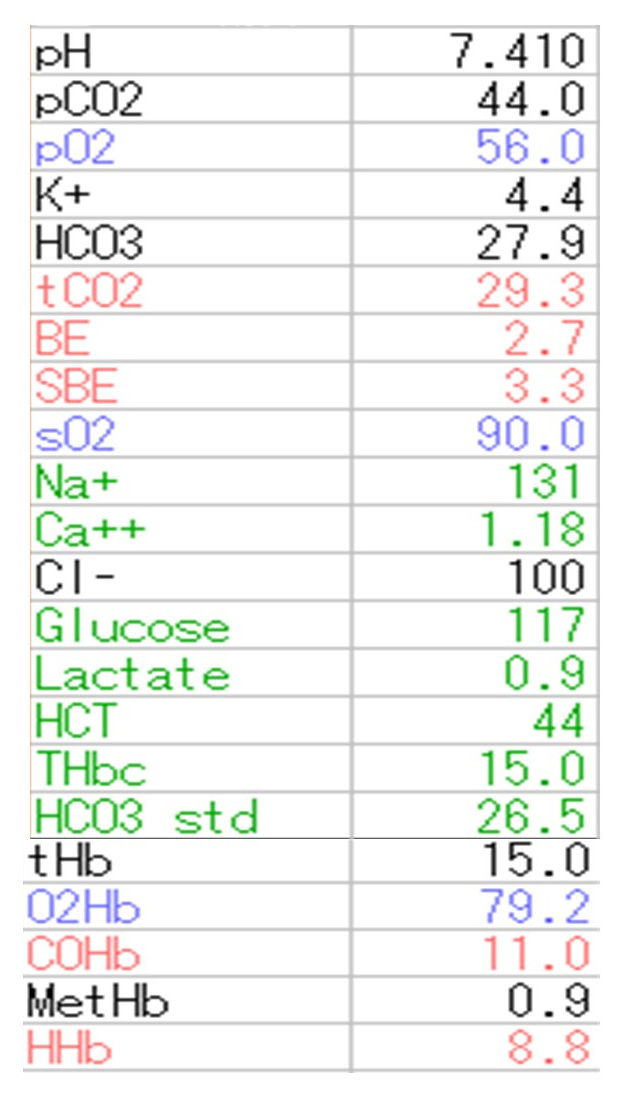
At the fifth visit, the patient’s blood gas results revealed COHb levels of 11.0%. The patient did not use a charcoal or oil heater. However, as a current smoker (20 cigarettes per day), he repeatedly smoked in a room without ventilation. This, together with the clinical situation, led to the diagnosis of CO poisoning. A review of his past blood results showed that although blood gas analysis had been performed as part of the routine examination on previous visits, high COHb levels (6.8−7.1%) were overlooked each time (Fig. 1).
Smoking cessation and staying in well-ventilated areas were recommended. There has been no recurrence of symptoms or ER visits following this advice.
Figure 1. Display of blood gas data obtained in our hospital. Non-routine variables such as carboxyhaemoglobin (COHb), methaemoglobin (MetHb) and HHb are also routinely displayed in our blood gas analyser
DISCUSSION
There were 3 reasons for the misdiagnosis in this case: first, the symptoms of CO poisoning were nonspecific; second, the patient had psychiatric disorders and third, the patient’s medical history was not thoroughly reviewed. Misdiagnosis of CO poisoning is common due to nonspecific symptoms such as headache, nausea and vomiting, fatigue and dizziness [1]. CO poisoning may be misdiagnosed as influenza viral infection because of the similarity between their symptoms [2]. There are also cases wherein CO poisoning was misdiagnosed as stroke, seizure, encephalitis or ischaemic heart disease [3]. The characteristic cherry-red appearance of the lips and skin is not observed in many cases of CO poisoning and is not useful for diagnosis. Thus, it is difficult to diagnose CO poisoning alone based on symptoms and physical findings. The second reason for misdiagnosis, in this case, was that the patient had multiple psychiatric disorders. Patients with psychiatric disorders are prone to psych-out errors, owing to which serious illnesses can be misdiagnosed [4]. On retrospective evaluation, the COHb levels were high in this case. However, the doctor did not confirm this test result. Consequently, a confirmation bias of ignoring contrary data occurred [4].
Third, there was a failure in obtaining the patient history thoroughly. When studying medical history, physicians are expected to imagine the events in a way that they can be "recreated" on video [5]. In our case, it would not have been difficult to diagnose CO poisoning if the doctor examining the patient could reproduce the mental imagery of heavy smoking in an enclosed space by enquiring about the patient's medical history in greater detail.
It may be difficult to obtain an accurate medical history from a patient with a psychiatric disorder. Physicians must make every effort to reconstruct the history as accurately as possible, using data collected from the patient, their next of kin or even from the discoverer. When patients with psychiatric disorders have nonspecific symptoms, it is necessary to check for the presence of an urgent underlying condition, including CO poisoning.