ABSTRACT
Hypotension in patients with heart failure is much more frequent in daily clinical practice than the 10–15% reported in clinical trials. In patients with heart failure with reduced ejection fraction (HFrEF), hypotension frequently limits the initiation and up-titration of guideline-directed medical therapy (GDMT). Midodrine is a peripheral alpha-1 agonist and a vasopressor anti-hypotensive agent approved for the treatment of orthostatic hypotension. We describe two cases where midodrine was prescribed in patients with HFrEF and hypotension.
LEARNING POINTS
- Hypotension in patients with systolic heart failure is a frequent presentation and can limit the initiation and optimization of guideline-directed medical therapy.
- Midodrine is a peripheral alpha-1 agonist and anti-hypotensive agent approved for the treatment of orthostatic hypotension.
- Midodrine may be used off-label in patients with heart failure with reduced ejection fraction (HFrEF) and symptomatic hypotension to allow optimization of medical therapy.
KEYWORDS
Midodrine, heart failure, noradrenaline
INTRODUCTION
AHypotension in patients with systolic heart failure is commonly seen during hospitalization, especially in those requiring haemofiltration for deteriorating renal function and volume overload. These patients usually need intravenous vasopressors to maintain blood pressure and consequently weaning them from intravenous support becomes a challenge. Midodrine exerts its action via activation of the alpha-adrenergic receptors of the arteriolar and venous vasculature to produce an increase in vascular tone and elevation in blood pressure. We report the cases of two patients with heart failure and difficulty being weaned from intravenous vasopressors where the introduction and slow titration of oral midodrine was successful in effecting intravenous vasopressor discontinuation.
Case 1 Description
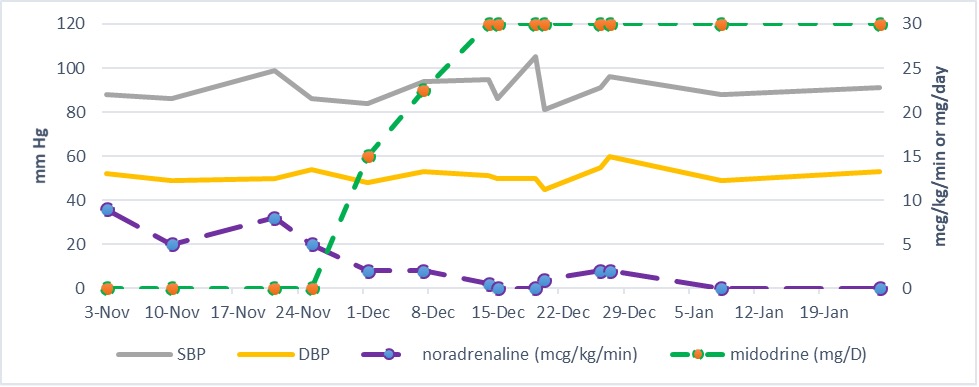
An 81-year-old female patient with a history of chronic cor pulmonale and pulmonary hypertension, chronic atrial fibrillation, obstructive sleep apnoea, bioprosthetic aortic valve replacement due to aortic stenosis, heart failure with preserved systolic function, and chronic kidney disease had been repeatedly admitted to hospital with exacerbation of right-sided heart failure that was frequently associated with low blood pressure. During her last admission, in order to support her blood pressure and maintain urine output, she received an intravenous (IV) noradrenaline infusion in variable doses and optimized diuretic therapy. However, her kidney function deteriorated and she became significantly overloaded and required haemofiltration sessions. The need for IV noradrenaline infusion persisted and several attempts to wean the patient failed due to a drop in blood pressure. After almost 21 days, midodrine was started in an attempt to wean her off IV support. The starting dose was 5 mg three times daily. After 5 days, it was noticed that noradrenaline requirements were higher on dialysis days so the dose was increase to 7.5 mg three times daily on dialysis days. A dose of 5 mg three times daily was maintained on off-dialysis days. The dose was ultimately increased to 10 mg three times daily on both on- and off-dialysis days and subsequently noradrenaline was successfully discontinued several days after midodrine was started (Fig. 1). Haemodialysis was conducted subsequently without the need for intravenous support. No major adverse events were observed during treatment.
Figure 1. The impact of titration of midodrine dose on noradrenaline requirement in a patient with heart failure and refractory hypotension.
DBP, diastolic blood pressure; HR, heart rate; SBP, systolic blood pressure
Case 2 Description
A 79-year-old male patient with a known history of ischaemic cardiomyopathy and advanced biventricular heart failure was frequently admitted to hospital with symptoms of heart failure and low blood pressure that limited drug titration and the initiation of guideline-directed medical therapy (GDMT) for class I heart failure. In his last admission he required both IV inotropic agents (dobutamin and levosimendan) and a vasopressor (noradrenaline) to support stroke volume and urine output. Despite this inotropic support, the patient’s blood pressure remained low with deterioration of renal function and volume overload. Haemofiltration sessions were started with IV noradrenaline support to maintain blood pressure. The need for IV noradrenaline persisted even in the off-dialysis days. To facilitate weaning off noradrenaline and possibly the initiation of GDMT for heart failure, oral midodrine 2.5 mg three times daily was started and slowly titrated with good tolerance to 10 mg three times daily. Gradually the dose of IV noradrenaline was decreased and the patient was successfully weaned over 3 weeks. Haemodialysis sessions were later tolerated well without the need for IV support. Small doses of GDMT were gradually administered and well tolerated.
DISCUSSION
Hypotension in patients with heart failure is much more frequent in daily clinical practice than the 10–15% reported in clinical trials [1]. In patients with heart failure with reduced ejection fraction (HFrEF), hypotension frequently limits the initiation and up-titration of GDMT mainly for class I indication [2]. It has been established that in acute heart failure a systolic blood pressure (SBP) below 90 mmHg is associated with poor outcome [3]. The main mechanisms that determine blood pressure components (systolic, diastolic and mean blood pressure) in patients with HFrEF are total blood volume, left ventricular stroke volume and peripheral vasodilatation [4].
Midodrine is a prodrug acting as an alpha-adrenergic agonist with rapid and near complete bioavailability which reaches 93% after oral administration. It exerts its action via activation of the alpha-adrenergic receptors of the arteriolar and venous vasculature to produce an increase in vascular tone and elevation in blood pressure [5]. The side effect profile is generally mild and dose-dependent. The Food and Drug Administration (FDA) in the USA approved the use of midodrine for the treatment of dysautonomia and orthostatic hypotension.
Midodrine has been used off-label in several small studies to prevent intradialytic hypotension (IDH). A systematic review conducted by Prakash et al. in 2004 showed six of 10 studies reported that midodrine improved IDH in haemodialysis patients [6]. On the other hand, in 2018 Brunelli et al. studied the impact of midodrine on outcomes in patients with IDH and concluded that midodrine administration was associated with higher rates of hospitalization, cardiovascular hospitalization and mortality [7].
Off-label use of midodrine in patients with heart failure and reduced systolic function is occasionally reported in the literature, but prevalence in this patient population is unknown. In a retrospective cohort study, Scoma et al. looked at the prevalence of midodrine use in systolic heart failure patients between January 2019 and December 2019. A total of 3,640 patients with decompensated HFrEF met the criteria and were included. Of these, 340 patients (9.3%) were prescribed midodrine to overcome hypotension as inpatients or just before discharge. GDMT such as beta-blockers, angiotensin receptor neprilisin inhibitor (ARNI) and mineralocorticoid receptor antagonists (MRA) were more likely to be prescribed to patients who were on midodrine when compared with those who were not. However, the increased use of GDMT in patients using midodrine did not improve prognosis. The authors concluded that midodrine was very commonly used in HFrEF patients, especially those with severely reduced left ventricular ejection fraction (LVEF), but noted a worse prognosis in this patient population [8].
Zakir et al. demonstrated in a small cohort study that the use of midodrine was well tolerated in patients with advanced heart failure associated with hypotension and allowed for up-titration of GDMT in these patients which consequently led to an improvement in LVEF and clinical outcomes with a significant decrease in hospital admissions and total hospital days [9].
Another small prospective study showed the safety of midodrine in patients with systolic heart failure and symptomatic hypotension despite concerns regarding vasoconstriction, and also demonstrated a significant increase in LVEF and improved outcomes because the patients could receive optimal GDMT [10].
A group of authors examined the hypothesis that midodrine use may improve autonomic dysfunction and systolic blood pressure and consequently enhance optimization of GDMT in patients with HFrEF. Among a cohort of 160 patients with HFrEF who had recently been discharged from hospital and seen in a clinic within a week, 60 were found to have autonomic dysfunction, a systolic blood pressure (SBP) below 95 mmHg and to be intolerant of beta- blockers, ARNI and MRA. Administration of an average dose of midodrine of 20.7 mg over period of 7 weeks in these patients resulted in beta-blockers being initiated in 75% of patients, ARNI in 50% and MRA in 33%. The mean improvement in SBP was 8±4 mmHg. Side effects were seen in less than 5% of patients and were limited to headache, palpitations or jitteriness. The authors concluded that midodrine appears to be feasible and safe and enables GDMT in patients with HFrEF associated with autonomic dysfunction and hypotension [11].
A more challenging situation, even in the hospital setting, arises when a patient with severe congestive heart failure and low blood pressure requires dialysis. Bergman studied a small number of patients with end-stage renal disease on outpatient dialysis and symptomatic heart failure with low blood pressure who received midodrine before and during their dialysis sessions. All patients showed an increase in the lowest mean arterial pressure (MAP) during dialysis and in post-dialysis MAP. Symptoms of congestive heart failure also improved [12].
Our two case reports reflect frequent scenarios seen in daily practice when physicians face difficulties weaning hypotensive patient with advanced heart failure off intravenous vasopressors. Midodrine may be used off-label to help wean these patients and to maintain blood pressure for the initiation and possible up-titration of GDMT. Further research is needed to assess the effects of midodrine on long-term mortality and morbidity in this patient population.