ABSTRACT
A cholesterol granuloma is a benign lesion that can occur in various organs, mimicking other pathologies. We present the case of a 35-year-old man presenting with asymptomatic lung and pleural lesions which were suspected to be pulmonary tuberculosis but found to be cholesterol granuloma on biopsy. Cholesterol granulomas are a rare mimic of common lung pathology and should be considered in the differential diagnosis if the initial investigations are not informative.
LEARNING POINTS
- Pulmonary cholesterol granuloma is a benign lesion that radiologically mimics many sinister pathologies.
- The pathogenesis of pulmonary cholesterol granuloma remains obscure and extensive work-up is usually needed to rule out malignancy and infectious aetiology.
KEYWORDS
Pulmonary tuberculosis, invasive aspergillosis, type II diabetes, immunocompromised
INTRODUCTION
Cholesterol granuloma is a benign lung lesion, usually found incidentally, that manifests as a pulmonary nodule [1]. It presents as a granulomatous lesion and has been reported in different organs such as the lung, central nervous system, and kidneys [2,3]. Although the aetiology of cholesterol granuloma remains unclear, the widely accepted theory is that the lipids within the granuloma have an endogenous rather than a dietary origin [4].
CASE DESCRIPTION
A 35-year-old Nepalese man presented with an abnormal chest x-ray found on routine employment screening. The patient was referred for further work-up. He denied any complaints. He had no cough, shortness of breath, chest pain, fever or weight loss. He had never smoked. He had no past medical history, no history of tuberculosis, and no contact with sick persons. There were no prior surgeries. His family history was non-contributory, in particular, there was no history of tuberculosis or malignancy in his family. He had no recent history of travel. He worked as a mason and had no occupational exposure to chemicals. The review of systems was otherwise unremarkable.
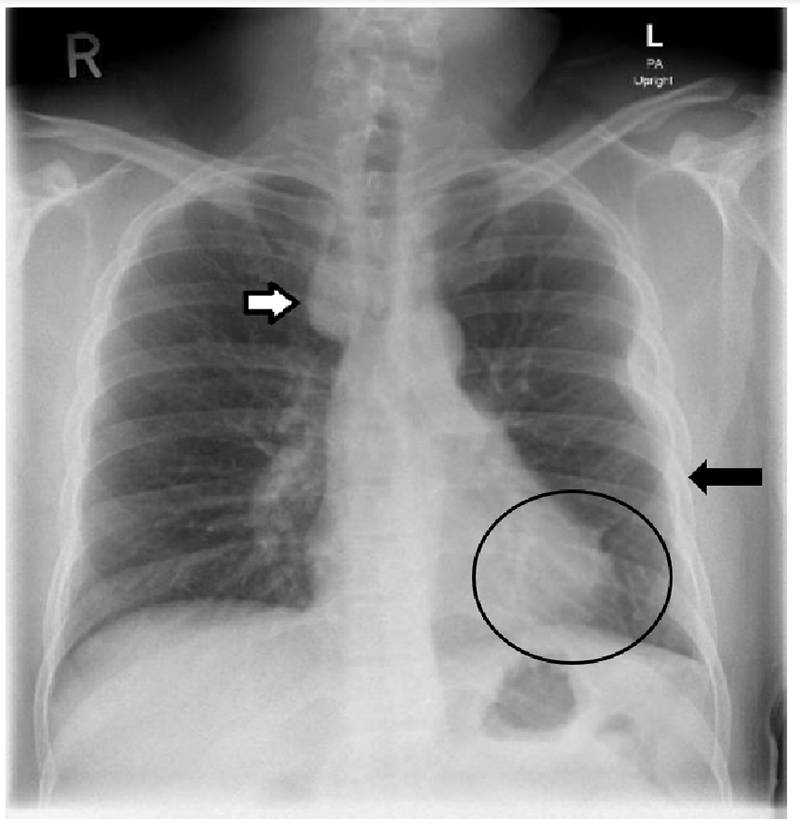
On physical examination, his vital signs including oxygen saturation on room air were within normal limits. A complete physical examination including respiratory examination showed no abnormal findings. He had normal laboratory investigations, with complete blood count, liver and renal parameters including calcium within normal ranges. He had no elevation of inflammatory markers including C-reactive protein. A chest x-ray showed a right paratracheal lesion (Fig. 1).
Figure 1. Chest x-ray showing right paratracheal well-defined mass lesion (white arrow), and pleural thickening in the left middle to lower lung zone (black arrow). Minimal atelectatic changes are noted in the left paracardial region with paracardial tenting (circle)
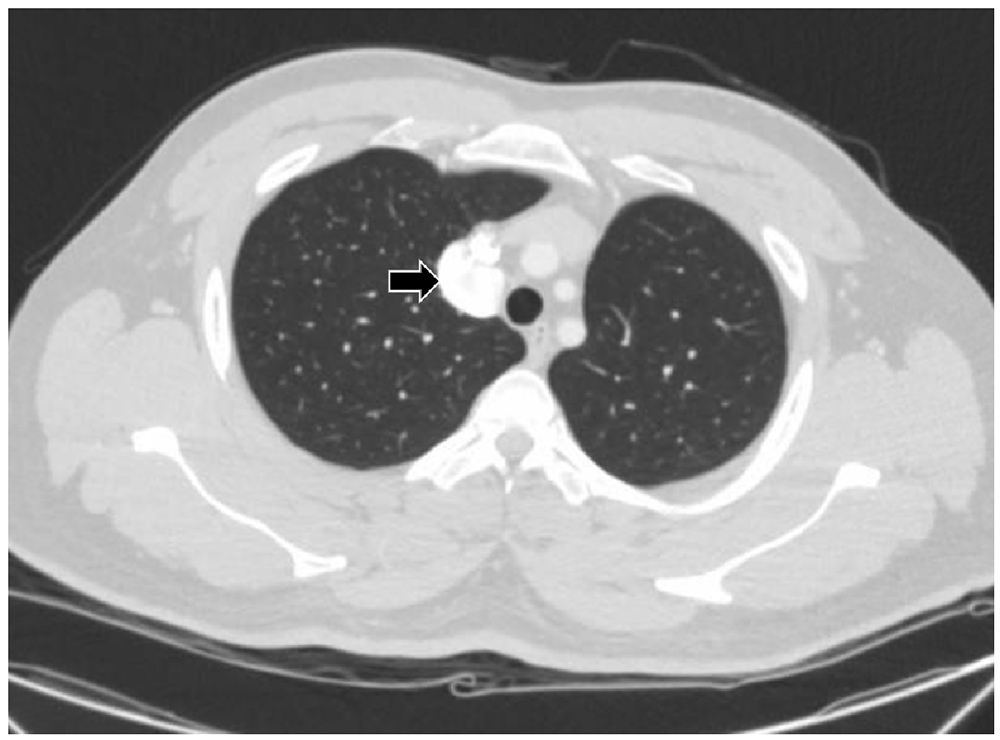
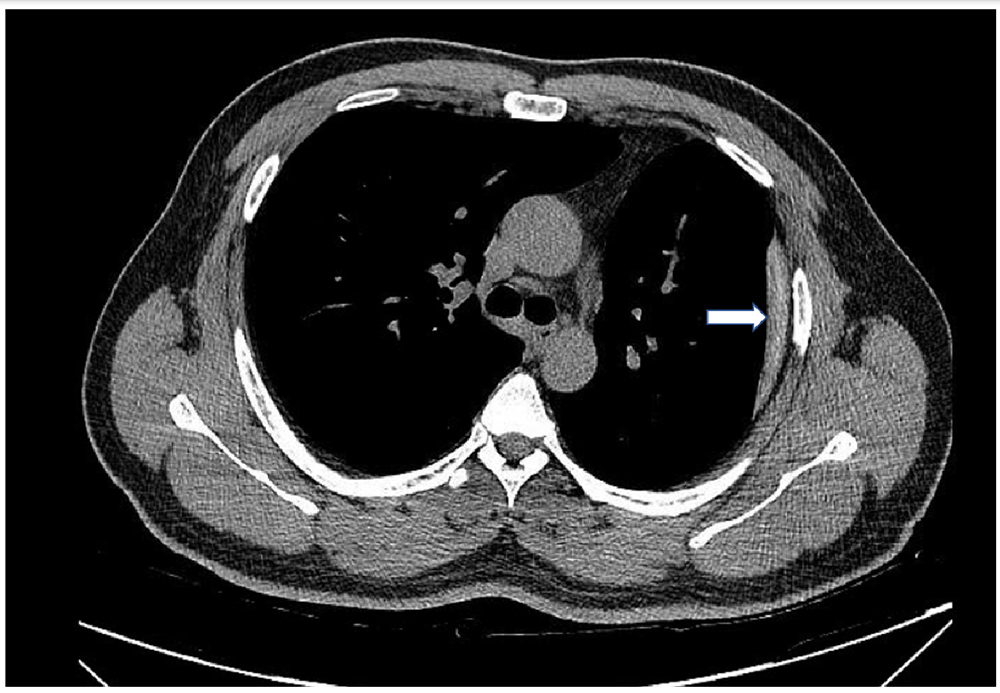
The patient underwent work-up for infectious aetiology including tuberculosis (TB) with two sets of acid-fast bacilli (AFB) smear, Xpert MTB/RIF assay and QuantiFERON, which were all negative. Further characterization of the paratracheal lesion was carried out via computed tomography (CT) of the chest which showed a mass of granulomatous aetiology (Figs. 2 and 3), as well as pleural plaques. Sputum and bronchoalveolar lavage for cytology and TB were negative. To further analyse the lesion, video-assisted thoracoscopic surgery was performed by the thoracic surgery team, with a biopsy from the pleural lesion confirming the diagnosis of cholesterol granulomas with calcifications.
Figure 2. CT of the chest showing a definite mass measured 2.4×3.4 cm in the right paratracheal area (arrow)
Figure 3. Pleural thickening (white arrow) and fibrotic stranding within the lateral basal segment of the left lower lobe was noted
The patient was diagnosed as having lung parenchymal cholesterol granuloma and discharged with follow-up in the outpatient clinic. On follow-up, he remained asymptomatic and did not require further intervention.
DISCUSSION
A case of pulmonary interstitial and intra-alveolar cholesterol granulomas associated with respiratory failure were diagnosed by biopsy and on autopsy, the patient believed to be an example of lipoid pneumonia coexisting with pulmonary alveolar proteinosis [5]. Moreover, pulmonary cholesterol granuloma has been assumed to be associated with pulmonary artery hypertension: as Nolan et al. reported in their study, five out of 20 patients with severe pulmonary hypertension were found to have cholesterol granuloma. However, our patient denied any symptoms, there was no evidence of pulmonary artery hypertension or respiratory failure, and the diagnosis was secured by histopathology. An extensive evaluation to rule out chronic infection was performed based on the patient's risks for pulmonary TB, radiological appearance, and our experience with atypical presentations of pulmonary TB in the region. Subsequently, obtaining a histopathological diagnosis of accessible tissue from the pleural lesions was warranted, which yielded the diagnosis of cholesterol granulomas.
The mechanism is not well understood but has been suggested to be related to surfactant degradation into phospholipids [6].
Radiologically, cholesterol granuloma findings are related to location, and the lesion may be more aggressive in appearance and extend to surrounding structures when it is located over bone, such as the petrous apex [7]. Pulmonary cholesterol granuloma presents as a centrilobular pulmonary nodule. It can also present as septal interlobular thickening ipsilaterally and small peripheral nodules in the contralateral lung in some patients [6,8]. The differential diagnosis is also location dependent: thrombosed internal carotid artery aneurysms and hydrated mucoceles have similar radiological characteristics [9]. Pulmonary nodules have many possible diagnoses, with the most serious being malignancy, which has to be ruled out. Our patient was at low risk of malignancy but was from a TB endemic area and so was investigated extensively [10]. Regarding management, cholesterol granuloma is a benign lesion, which if asymptomatic, requires follow-up to ensure lesion stability. However, symptomatic lesions require surgical removal [10,11]. In the patient presented here, who was asymptomatic, the only intervention required was biopsy at diagnosis. On further follow-up, the patient remained asymptomatic.
CONCLUSION
Pulmonary cholesterol granuloma is a benign pulmonary lesion that can be found incidentally. The diagnosis is challenging radiologically as it may not be well differentiated from infectious and malignant lesions. Therefore, clinical suspicion is important and cholesterol granulomas should be considered in the differential diagnosis of lung granulomas with non-infectious aetiology.