ABSTRACT
Introduction: Lymphangiomas are rare, congenital malformations arising from lymphatic hyperplasia. More than 90% of cases are found in children under 2 years of age. Cystic lymphangiomas usually occur in the neck and axillary region and only rarely extend to the mediastinum.
Case Description: We present the case of a middle-aged woman who presented with dyspnoea and productive cough. A chest x-ray showed right lower medial lung opacity, and a CT scan of the thorax showed a cystic mediastinal mass, encroaching on the superior vena cava and approaching the trachea and mainstem bronchus. An anterior thoracotomy with tumour resection was performed to relieve compression symptoms. The final pathology report confirmed the diagnosis of mediastinal lymphangioma.
Discussion: Lymphangioma should be considered as one of the differential diagnoses when mediastinal widening is found on chest x-ray, and it should be investigated further with a CT scan and biopsy. Infiltration of surrounding structures can cause compression symptoms and can also make surgical resection more challenging.
LEARNING POINTS
- Lymphangiomas are benign tumours of the paediatric population that can rarely occur in middle-aged adults as an acquired form.
- It is essential to investigate mediastinal enlargement seen on chest x-ray images even in the absence of any symptoms, as mediastinal lymphangiomas can grow to involve nearby anatomical structures.
- Although benign, lymphangiomas should be excised at the time of diagnosis to avoid anticipated complications and compression of anatomical structures causing respiratory difficulty, hoarseness and superior vena cava syndrome.
- Complete surgical resection is the mainstay of treatment and provides an excellent postoperative prognosis.
KEYWORDS
Lymphangioma, mediastinal mass, lymphatic system
INTRODUCTION
Lymphangiomas are rare malformations with cutaneous and mucous membrane manifestations due to lymphatic vessel hyperplasia. They commonly occur in children as congenital malformations, with more than 90% of cases observed in patients younger than 2 years of age [1]. Based on histological features, lymphangiomas are classified into the following: (1) lymphangioma simplex, (2) cavernous lymphangioma, and (3) cystic lymphangioma or cystic hygroma [2]. Cystic lymphangioma usually appears in the neck or the axillary region and rarely extends into the mediastinum; the latter accounts for 0.7–4% of all mediastinal tumours, and less than 30 cases have been reported in the literature in the last 23 years [3]. The majority of these tumours are silent, and the acquired type may be detected in middle-aged adults as an incidental finding on chest x-ray imaging [4]. However, patients with symptomatic tumours may present with respiratory difficulty, hoarseness and superior vena cava syndrome due to compression of adjacent structures. This study reports a rare case of adult-onset solitary mediastinal cystic lymphangioma in a female patient.
CASE DESCRIPTION
A 42-year-old woman with hypertension, obesity hypoventilation syndrome requiring 4 litres of supplemental oxygen, and a 20 pack-years smoking history, presented with worsening dyspnoea and productive cough for 2 weeks. On examination, she had hypertension (BP 150/96 mmHg), tachycardia (HR 112 bpm), and tachypnoea (RR 30) with oxygen saturation of 89% on 4 litres of supplemental oxygen. On auscultation, coarse rhonchi were heard in all lung fields bilaterally. The general physical examination was otherwise unremarkable.
Upon admission, the patient had already undergone extensive investigations at other hospitals over the years. Three years previously, chest computed tomography (CT) had shown a right-sided cystic mediastinal mass measuring 6.1×5.3×7.5 cm. She was presumptively diagnosed with a bronchogenic cyst, and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) removed 114 ml of cloudy pale fluid. Following the procedure, the size of the mass decreased, and the patient's clinical symptoms improved. The needle rinse and core tissue culture did not detect any growth, and the cytology reports showed small mature lymphocytes but no epithelial cells. One week before presentation at our hospital, the patient had a biopsy at another hospital of the cystic mediastinal mass which had enlarged once again, that showed paucicellular cells with rare histiocytes and proteinaceous debris consistent with a bronchogenic cyst.
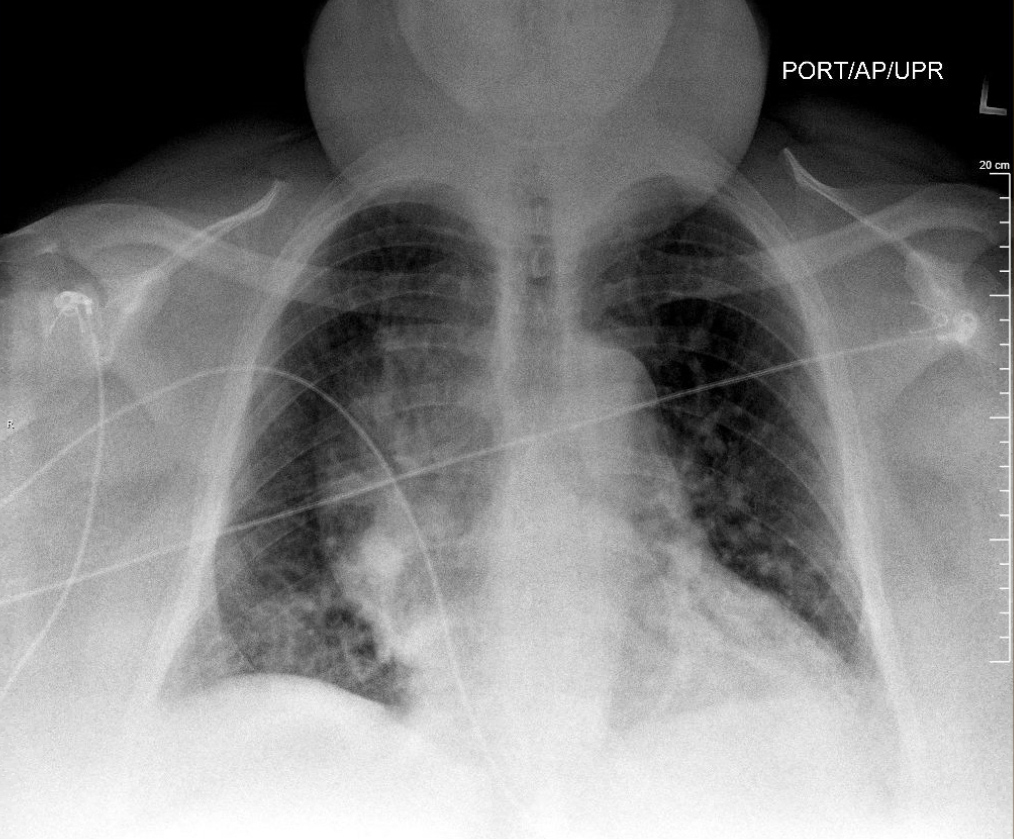
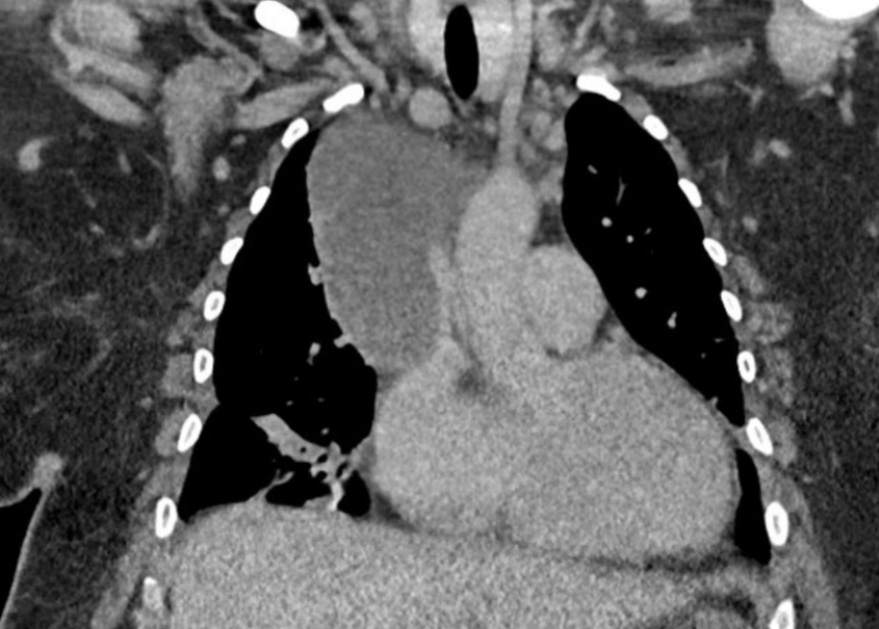
A chest x-ray (CXR) performed on the current presentation demonstrated significant right medial mid-lung opacity of low attenuation (Fig. 1). It was followed by a contrast-enhanced CT scan of the chest, which revealed a cystic mass measuring 9.5×6.5×9.0 cm in the right side of the mediastinum with simple fluid attenuation and no nodularity. In addition, the mass was abutting and mildly compressing the lower portion of the superior vena cava (Fig. 2). We looked into the patient’s old medical records and found a CXR from 12 years previously that did not show any cardiopulmonary process, signifying that the current clinical manifestation was an adult-onset pathological lesion.
Figure 1. Chest x-ray showing large right medial mid-lung opacity adjacent to the mediastinum and right lung border
Figure 2. CT images demonstrating a fluid attenuating mass in the right mediastinum extending from the level of the hilum superiorly to the right apex, with maximum axial dimensions of 9.5×6.5 cm and a craniocaudal length of 9 cm. The mass is abutting and mildly compressing the lower portion of the superior vena cava
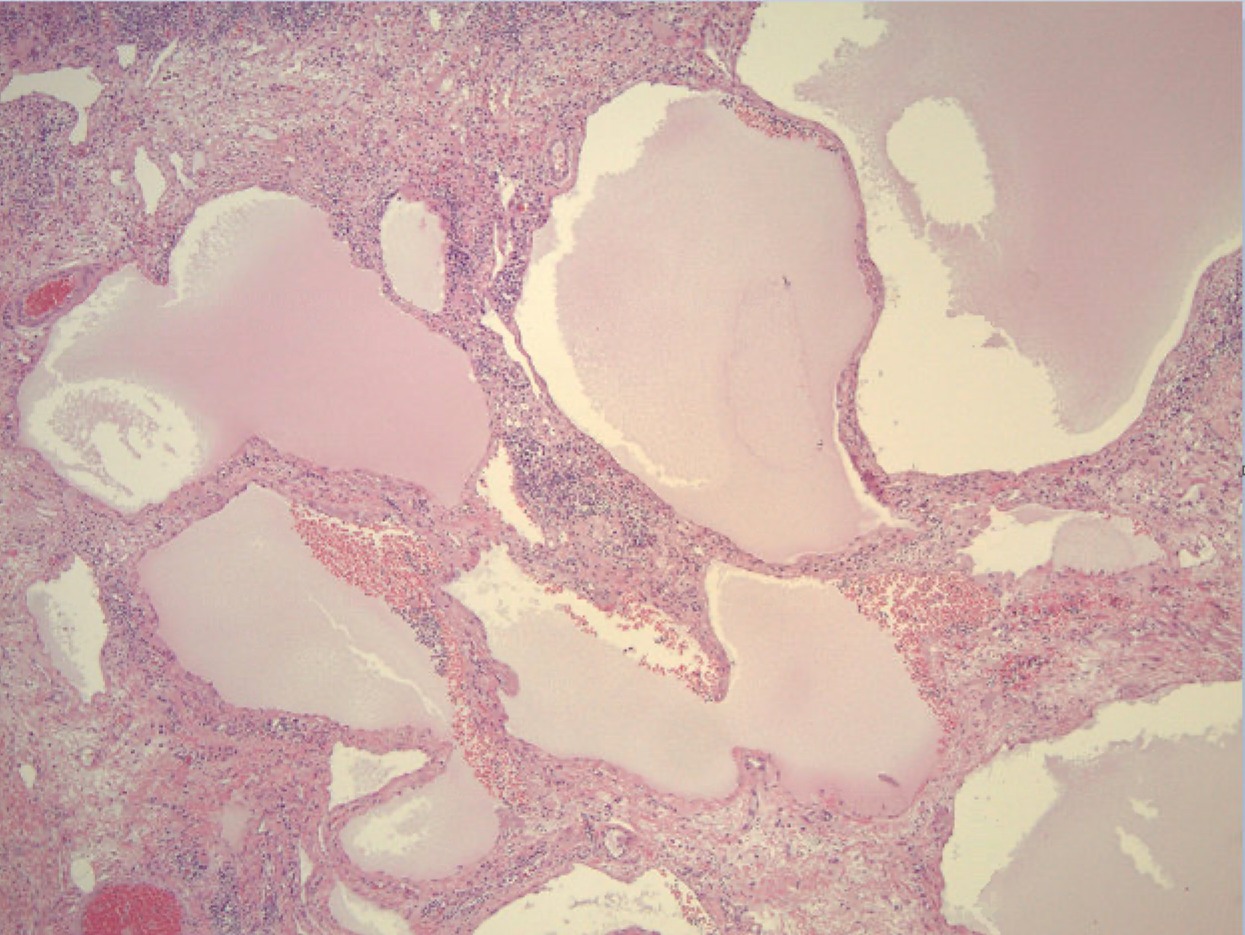
Following discussion between the pulmonologist and the cardiothoracic surgeon, surgical excision of the mediastinal mass was deemed necessary considering its large size, relapsing nature, and expansion towards surrounding structures. Anterior mediastinotomy and cystotomy was performed for cyst drainage and 250 ml of brownish fluid content was aspirated and sent for pathological examination. The cyst capsule was adherent to the superior vena cava and multiple vessels in the mediastinum, requiring extensive dissection and wide drainage of pleural and mediastinal space. Sections of the capsule sent for pathology revealed multilocular cystic structures lined by indiscernible to flat endothelial cells filled with lymphatic fluid. The wall also contained lymphoid tissue (Fig. 3). The lymphatic endothelial lining cells were highlighted by positive immunostaining of the monoclonal antibody D2-40, CD31, and ERG oncoprotein expression. The combined morphological features and immune profiles were most consistent with cystic mediastinal lymphangioma. The patient’s dyspnoea and hypoxaemia improved after surgery and she was able to saturate well at her baseline oxygen requirement. The patient was counselled regarding the benign but recurring nature of the mass, as well as the need for regular follow-up.
Figure 3. Histology slide demonstrating multilocular cystic structures lined by flat endothelial cells and filled with lymphatic fluid. The wall contains lymphoid tissue
DISCUSSION
Mediastinal lymphangioma is extremely rare in adults; the final diagnosis of this acquired form may be delayed until surgical exploration and histoimmunopathological examination and characterization. It may be detected as an incidental mass on CXR causing mediastinal widening, after which further imaging and biopsy are necessary. The most common and established CT features of mediastinal lymphangioma include a well-circumscribed lesion without calcifications and variations in attenuation values within the lesion. These features augmented by MRI findings can aid in determining disease extent and guide therapy. Despite a lack of consensus on lymphangioma management between observation and surgical resection, the latter remains the mainstay of treatment. Most physicians agree that the tumour should be excised at the time of diagnosis to avoid the danger of complications and compression of nearby anatomical structures causing symptoms of respiratory difficulty, hoarseness and superior vena cava syndrome [4]. Complete surgical resection provides an excellent postoperative prognosis. However, some adverse events, including local infections, fistula formation and recurrences, have been reported [5]. Chemotherapy, radiotherapy and sclerotherapy are alternative treatments with varied results that could be useful if large tumour size or multiple loculations makes a surgical approach impossible.