ABSTRACT
Background: Chyluria is usually associated with parasitic disease caused by Wuchereria bancrofti and is rare in non-endemic regions. The management of chyluria varies according to the severity of the condition. This report describes a case of mild chyluria and successful treatment using sclerotherapy.
Case description: A 44-year-old man presented with a first episode of painless milky urine. The diagnosis of chyluria was established following retrograde pyelography showing a fistula between the right pelviocalyces and the retroperitoneal lymphatic systems. The patient had not travelled to any endemic regions. Sclerotherapy using povidone-iodine was carried out resulting in closure of the fistula.
Conclusion: Sclerotherapy using povidone-iodine as the sclerosing agent was effective and safe for the management of a patient with mild chyluria. However, the best treatment for chyluria should be tailored to the patient’s condition.
LEARNING POINTS
- Treatment of chyluria with instillation of povidone-iodine as a sclerosing agent provides an excellent outcome.
- The treatment of chyluria is should be tailored to disease severity.
KEYWORDS
Chyluria, management, sclerotherapy, povidone-iodine
INTRODUCTION
Chyluria is a rare condition caused by leakage of lymphatic fluid into the pelviocalyces system and characterized by the presence of chyle in the urine, giving it a milky appearance. The condition is usually associated with filariasis, which is rare in non-endemic regions and may block lymphatic drainage. Chyluria is classified as mild, moderate or severe, according to clot frequency, amount of weight loss, and calyx involvement seen on pyelography [1]. The diagnosis of chyluria is usually based on the presence of milky urine with an additional test to detect chylomicrons in the urine. Although it has poor sensitivity, intravenous pyelography is commonly used to identify the location of the fistula. There are several management approaches ranging from conservative therapy to surgical intervention [2]. This report describes a healthy man with chyluria who lived in a non-endemic area.
CASE DESCRIPTION
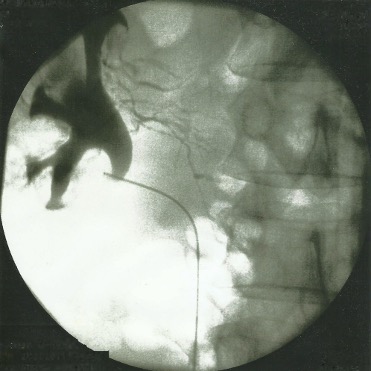
A 44-year-old man presented with a first complaint of milky urine 2 days before admission. He had no history of major disease. Complete blood and urine examinations were carried out. Haematological results were within normal limits with a normal total albumin level. Urine analysis revealed sterile urine. Cystoscopic evaluation ruled out efflux from both ureteral orifices. Retrograde pyelography subsequently performed on both kidneys demonstrated a fistula between the right pelviocalyces and the retroperitoneal lymphatic systems as shown by pelviocalyces-lymphatic reflux (Fig. 1). A 5 Fr ureteral catheter was left in place and positioned so the proximal tip of the catheter was inside the right pelviocalyces system. The distal part of the ureteral catheter was attached to a 16 Fr Foley catheter. A mixture of 10% povidone-iodine was instilled into the right pelviocalyces system twice a day for 2 days. Retrograde pyelography at the end of treatment did not show any communication between the right pelviocalyces and left retroperitoneal lymphatic systems. The patient was discharged with oral antibiotics and analgesics for another 3 days.
DISCUSSION
Chyluria is a condition where chyle is present in the urine, turning it a milky colour. Chyle is a mixture of fat, proteins and fibrin. Depending on aetiology, chyluria is classified as parasitic or non-parasitic [3]. Endemic areas for the disease include India, Japan, China, sub-Saharan Africa, Southeast Asia and South America, where Wuchereria bancrofti is usually the causative parasite. Non-parasitic causes include malignancy, infection, trauma and congenital anomalies. Chyluria is caused by obstruction of the retroperitoneal lymphatic system that eventually drains its contents into the urinary system, which leads to the development of fistulas in the pelviocalyces, ureter, bladder or urethra, with the pelviocalyces being most common site. Symptoms of chyluria vary from just the passage of milky urine to ureteral colic due to clot formation by the chyle. Patients with severe chyluria may present with significant weight loss, malnutrition and immunosuppression [4]. The current report has described a non-parasitic cause of chyluria as the patient had not travelled to any endemic areas during the previous 5 years and there were no reports of any disease in the region where the patient lived.
The grading of chyluria severity depends on presentation: grade 1 if the patient complains of milky urine, grade 2 if there are episodes of clot retention, and grade 3 if there is an episode of haematochyluria [5]. The diagnosis of chyluria is based on urine and blood analysis, imaging, and immunological examination [2]. On urine examination, milky chylous urine is evident and may contain fibrin and chylomicrons. Blood analyses usually shows eosinophilia and if patients have severe chyluria, they may also have albuminaemia due to protein drainage to the urinary system. Retrograde pyelography and intravenous pyelography are used to locate the fistula between the lymphatic and urinary systems. The patient in this study had mild chyluria because he did not complain of urinary retention due to the disease.
There are several management approaches depending on disease severity. Conservative treatment is applied in patients with mild chyluria and may include dietary restriction of triglycerides and medications including diethylcarbamazine, albendazole and ivermectin. Sclerotherapy is usually used in patients not responding to conservative management. Instillation of a sclerosing agent at the site of the fistula can cause the fistula to close. Commonly used sclerosing agents include povidone-iodine, dextrose, silver nitrate, hypertonic saline or a combination of these agents [6]. Surgical management is recommended in patients not responding to previous approaches, who are therefore considered to have refractory chyluria.
Surgical treatment includes chylolymphatic disconnection, lymphovenous anastomosis, autotransplantation and nephrectomy on the affected side [2]. This study has described a patient with mild chyluria who was suitable for conservative management but underwent sclerotherapy because the ureteral catheter used to deliver the sclerosing agent had already been placed for retrograde pyelography.
CONCLUSION
The management of chyluria varies depending on disease severity. This study has reported that the instillation of 10% povidone-iodine as a sclerosing agent into the pelviocalyces system was an effective and safe treatment in a healthy patient with chyluria.