ABSTRACT
Hemosuccus pancreaticus (HP) is defined as bleeding from the ampulla of Vater through the pancreatic duct. It is a rare complication associated with acute or chronic pancreatitis. The source of bleeding can be from the pancreas itself or surrounding vessels, with the splenic artery most commonly involved. Diagnosing HP is challenging and computed tomography angiography remains the gold standard for diagnosis. We present the case of a 62-year-old male with recurrent pancreatitis complicated with HP. Imaging and endoscopy were consistent with bleeding from the section portion of the duodenum, which resolved without intervention.
LEARNING POINTS
- Hemosuccus pancreaticus is a rare complication associated with acute or chronic pancreatitis.
- CT angiography is the gold standard for diagnosing hemosuccus pancreaticus.
- Arterial embolization is the first-line treatment of hemosuccus pancreaticus.
KEYWORDS
Pancreatitis, hemosuccus pancreaticus, upper gastrointestinal bleeding, arterial embolization
CASE DESCRIPTION
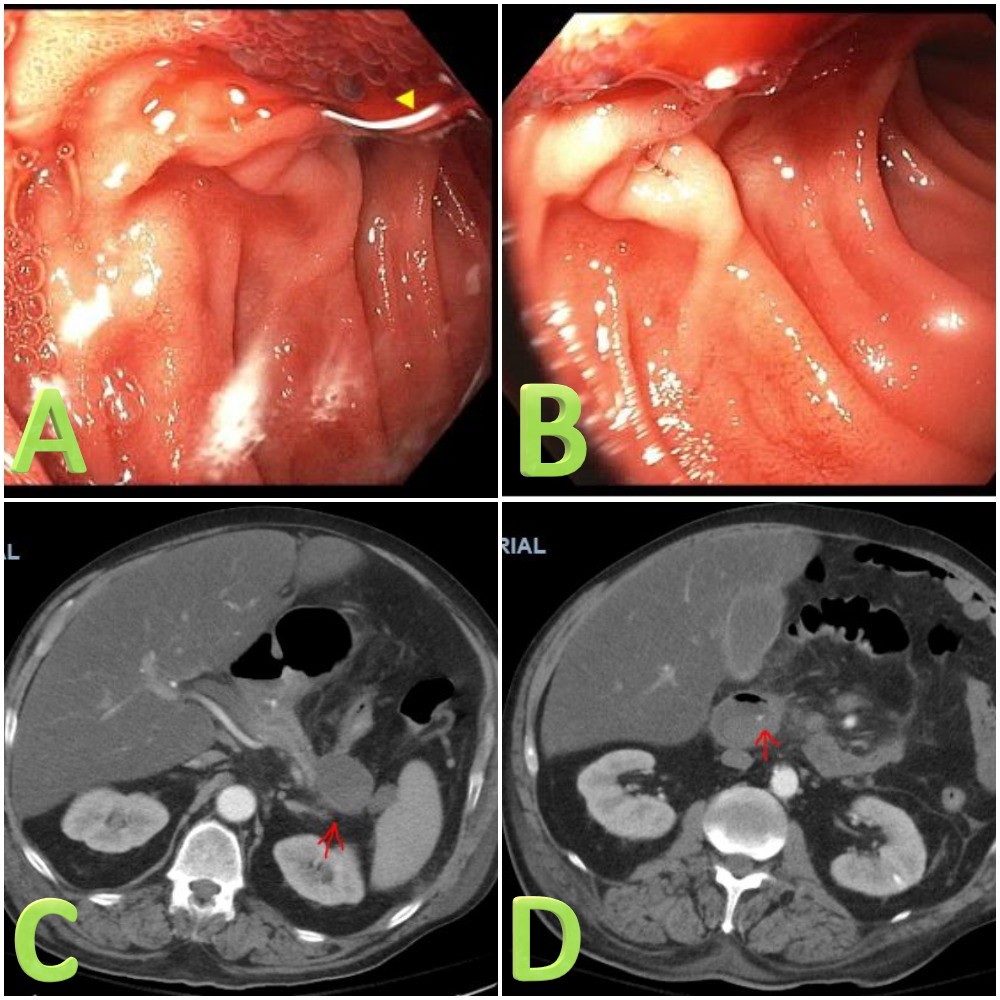
A 62-year-old Caucasian male with a history of recurrent pancreatitis and alcohol dependence presented with a sharp and diffuse abdominal pain associated with nausea, vomiting, and one episode of melena. Laboratory tests were significant for elevated liver enzymes, total and direct bilirubin, lactic acid, and lipase. Computed tomography (CT) of the abdomen with contrast demonstrated acute pancreatitis with pseudocyst formation anterior to the tail of the pancreas measuring 4.5 x 3.5 cm. The patient was admitted for management of acute pancreatitis. On day 4, he reported multiple red bloody bowel movements and worsening abdominal pain. He also became hypotensive and tachycardic. His rectal exam was positive for maroon-colored blood. CT angiography of the abdomen revealed bleeding from the second portion of the duodenum. Esophagogastroduodenoscopy (EGD) revealed blood coming from the ampulla of Vater consistent with hemosuccus pancreaticus (HP) (Fig. 1). Interventional radiology was consulted; however, no active bleeding was found. The patient was transferred to the intensive care unit for close monitoring where his symptoms improved. His hemoglobin remained stable after receiving two units of packed red blood cells and no emergency surgery was required. The patient then decided to discharge himself against medical advice; however, he was readmitted 7 days later with alcoholic hepatitis complicated with ascites and spontaneous bacterial peritonitis. He continued to decompensate until he died, although there was no bleeding reoccurrence during his second hospitalization.
Figure 1. A and B: Blood oozing from the ampulla of Vater (arrow head). C: CT angiogram showing pancreatic pseudocyst formation at the tail of the pancreas. D: CT angiogram showing contrast in the second portion of the duodenum consistent with intraluminal hemorrhage
DISCUSSION
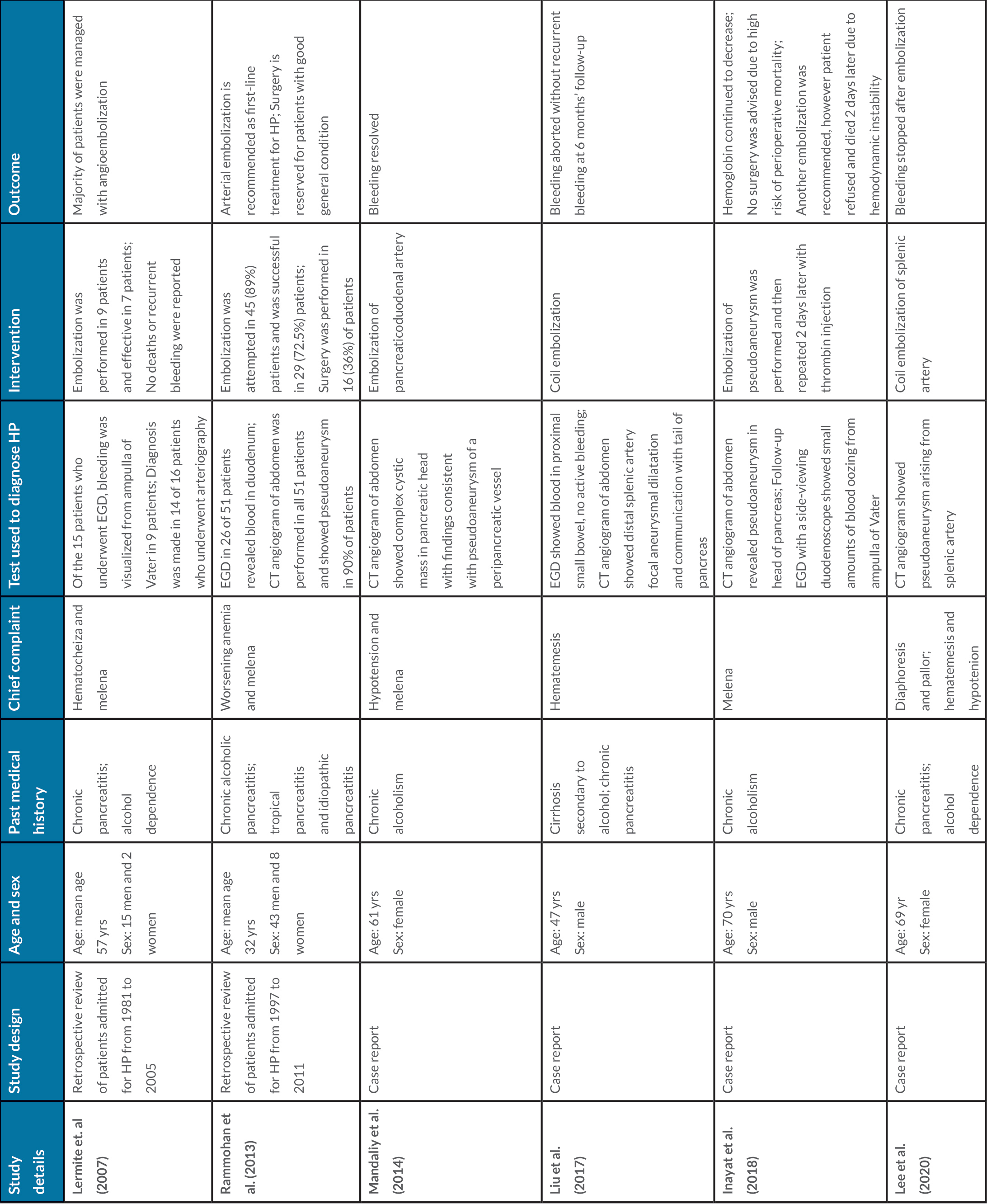
Hemosuccus pancreaticus (HP) is defined as bleeding from the ampulla of Vater through the pancreatic duct. The bleeding source can be the pancreas itself or arteries adjacent to it. During acute or chronic pancreatitis, pancreatic juices can corrode the peripheral vascular wall and cause an arterial aneurysm or pseudoaneurysm[1,2]. Common arteries reported are splenic, hepatic, gastroduodenal, or pancreaticoduodenal, with the splenic artery most commonly involved, as shown in Table 1[2–7]. As with our patient, HP can also result from a pancreatic pseudocyst due to its communication with the pancreatic duct, which can be intermittent due to clot formation in the main duct[1]. HP is usually diagnosed either via direct visualization of bleeding from the ampulla of Vater by endoscopy, which can detect active bleeding in only 30% of patients, or via CT angiography[1]. Blood tests usually do not show any significant abnormalities unless there is a concomitant episode of acute pancreatitis or alcoholic hepatitis, in which case there may be some elevation in liver enzymes and lipase as with our patient[1]. Lermite et al. reported that of 17 patients who underwent endoscopy, nine were diagnosed with HP by direct visualization of bleeding[3]. Alternatively, of 16 patients that underwent CT angiography, 14 were diagnosed with HP[3]. Similar results were reported by Rammohan et al., which explains why CT angiography remains the gold standard in diagnosing HP and therapy by angioembolization if possible[4]. Arterial embolization is the first-line treatment for HP, as shown in Table 1[2–7]. Surgical options are associated with higher mortality and rebleeding rates; therefore, surgery should be reserved for patients with active bleeding and those hemodynamically unstable[1]. In Rammohan et al., surgical intervention was attempted in 36% of patients to control bleeding after the failure of arterial embolization[4]. Some of the surgical procedures mentioned in that study were distal pancreatectomy and splenectomy, central pancreatectomy, and intracystic blood vessel ligation[4]. In our case, initial angiography did not show active bleeding and therefore no surgical intervention was required.