ABSTRACT
Cholecystogastric fistulas are a rare but life-threatening complication of cholelithiasis. This medical condition has been explained in detail in several cases in the medical literature. However, there is still conflicting debate on how well to effectively manage patients with such a complex medical condition. We present a 70-year-old Caucasian female with complaints of intermittent dull non-radiating abdominal pain. Her pain started abruptly after breakfast. Patient took some acetaminophen which alleviated her symptom. Several days later, pains return but at this time it was associated with constipation. Patient’s primary care physician (PCP) suspected peptic ulcer disease, which was quickly ruled out following negative result of Helicobacter pylori breath test. The PCP advised patient to visit the emergency department for further investigations to rule out/in possible gallstone ileus causing intestinal obstruction, or Bouveret’s syndrome.
LEARNING POINTS
- Native triple-valve endocarditis is extremely rare, especially in the absence of predisposing conditions.
- Streptococcus gallolyticus has been associated with endocarditis as well colonic and hepatobiliary pathology, so gastrointestinal endoscopy is important as bacteraemia frequently precedes gastrointestinal symptoms, allowing prompt diagnosis.
- In multivalvular involvement, early surgery is often required, and timely recognition and treatment before complications develop may be decisive for prognosis.
KEYWORDS
Peptic ulcer, gallstone ileus, cholecystogastric fistula, intestinal obstruction, Bouveret’s syndrome
INTRODUCTION
Cholecystogastric fistulas are a rare but life-threatening complication of cholelithiasis. Despite several cases described in the medical literature, there is ongoing debate on how to effectively manage these patients and their complex condition. According to the Centers for Disease Control and Prevention (CDC), cases of non-injury visits to the emergency department (ED) for which abdominal pain was the chief complaint increased by 31.8% from 5.3 million in 2000 to 7.0 million in 2008, constituting a 7.6% rise during this time, and continue to rise[1]. Small bowel obstructions account for 2% of all patients presenting to the ED with abdominal pain[2]; they have different etiologies, with the most common being tissue adhesions from previous abdominal surgeries, followed by hernias[3]. We present a case of abdominal pain secondary to gallstone ileus, a rare cause of bowel obstruction.
CASE DESCRIPTION
A 70-year-old Caucasian female presented to the ED with abdominal pain. She had a 2-day history of intermittent dull abdominal pain, constipation, and dysuria. Over-the-counter laxatives appeared to alleviate the constipation at the time; however, when her symptoms got worse she met with her primary care physician. She denied any nausea or vomiting. Her past medical history was negative for surgery and she denied using tobacco, alcohol, or illicit drugs. Her family history was non-contributory. The primary care physician ordered a plain abdominal X-ray, which suggested a small bowel obstruction, and immediately advised her to visit the ED for further evaluation.
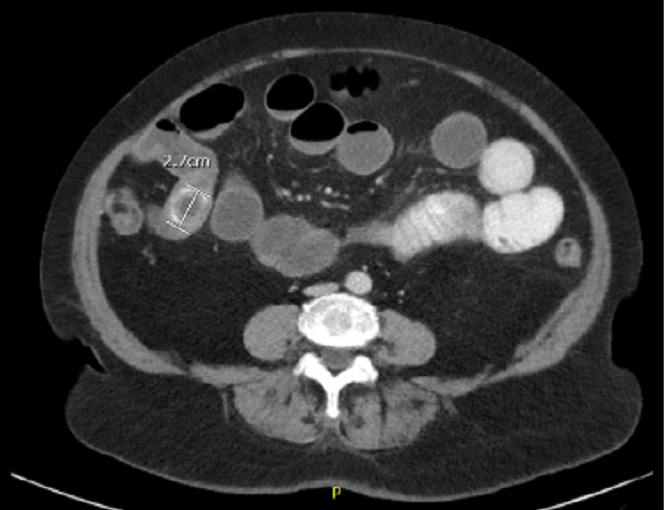
Physical examination revealed mild pain upon palpation of the entire abdomen. A computed tomography (CT) scan of the abdomen and pelvis with both intravenous (IV) and oral (PO) contrasts revealed a 2.7 cm gallstone in the terminal ileum with dilated loops of the small bowel in the right lower quadrant, indicative of gallstone ileus (Fig. 1).
Pneumobilia was equally evident with PO contrast in the contracted gallbladder, suggestive of a cholecystogastric fistula (fistula between the gallbladder and gastric antrum) (Fig. 2).
Figure 1. Contrast-enhanced CT scan of a cross-sectional view of the abdomen showing a gallstone at the ileocecal junction with pneumobilia present
Figure 2. CT scan with PO contrast of an axial section of the abdomen showing a 2.7 cm gallstone with resultant dilated fluid-filled loops of the small bowel suggestive of a small bowel obstruction
Peptic ulcer with perforation was subsequently ruled out given the PO contrast scan result in addition to the lack of peptic ulcer clinical symptoms in our patient.
A general surgery consultation was obtained. The patient was treated with a nasogastric tube and IV fluids and admitted to the general ward. Some hours after symptomatic treatment, the patient developed severe abdominal pain with worsening of symptoms and was immediately transferred to the operating room for an exploratory laparotomy with manual extraction of the stone by assisted enterotomy. On postoperative day 1, she was able to pass flatus, while on day 2 she had a bowel movement. She made a good recovery and it was decided to defer performing a cholecystectomy.
DISCUSSION
Adhesions continue to be the most common cause of small bowel obstruction, as noted previously[3]. Gallstone ileus is a rare condition; the incidence is approximately 0.095% of all causes of mechanical bowel obstruction. Most commonly, gallstone ileus affects elderly females[4]. Unfortunately, patients with gallstone ileus often present with vague complaints. It is common to experience symptoms of episodic abdominal pain due to the dislodged gallstone, which intermittently/partially blocks the cystic duct until completely blocked[5]. Some patients complain of nausea and vomiting, while others have more severe symptoms. The most common distal site of obstruction is the ileocecal junction[6]. However, gallstones can obstruct any part of the intestinal tract, including the proximal gastric outlet, a phenomenon known as Bouveret’s syndrome[7].
When gallstone ileus is diagnosed in a patient, it is imperative to thoroughly examine the entire biliary tree to identify the exit point of the gallstone. Common pathways of gallstones exiting the gallbladder due to fistula formations include cholecystoduodenal (75%), cholecystocolonic (10–20%), and cholecystogastric (5%)[8].
Chronic cholecystitis is the main cause of fistula formation[9]. The definitive treatment for fistula formation is surgery, during which a manual extraction of the gallstone with an assisted enterotomy is performed, with either cholecystectomy and fistula closure, a bowel resection, or a bowel resection with fistula closure[10]. However, most cases of fistula formations are treated with enterotomy and stone extraction alone. No randomized clinical control trials have evaluated these options to date, most likely due to its low incident rate.
CONCLUSION
Although cholecystogastric fistula is a rare, life-threatening complication of gallstone ileus in the elderly, surgical closure of the fistula is not always necessary.
The choice of surgical intervention needs to be determined based on the patient’s clinical presentation and intraoperative evaluation. Several cases in the literature have suggested that cholecystostomy with enterolithotomy followed by cholecystectomy with fistula closure (with the latter performed only when the patient’s condition completely improves) are adequate treatment for preventing early biliary pathology recurrence. However, our patient recovered fully following a laparotomy without excision of the fistula nor cholecystectomy and had an uncomplicated postoperative course. In summary, a cholecystogastric fistula can be effectively managed with improved surgical techniques and use of laparoscopic surgery, which can lead to a positive outcome, as in our patient’s case.