ABSTRACT
Infective endocarditis is a condition associated with high morbidity and mortality, usually with univalvular involvement. We describe the case of a 76-year-old woman with triple-valve endocarditis due to Streptococcus gallolyticus, complicated by perivalvular suppurative lesions, acute heart failure and acute kidney injury. Unfortunately, the patient died despite antibiotic therapy and emergent surgery. This case highlights uncommon triple-valve involvement in the absence of risk factors, posing a diagnostic and therapeutic challenge.
LEARNING POINTS
- Native triple-valve endocarditis is extremely rare, especially in the absence of predisposing conditions.
- Streptococcus gallolyticus has been associated with endocarditis as well colonic and hepatobiliary pathology, so gastrointestinal endoscopy is important as bacteraemia frequently precedes gastrointestinal symptoms, allowing prompt diagnosis.
- In multivalvular involvement, early surgery is often required, and timely recognition and treatment before complications develop may be decisive for prognosis.
KEYWORDS
Triple-valve endocarditis, Streptococcus gallolyticus, infective endocarditis
CASE DESCRIPTION
A 76-year-old woman with history of arterial hypertension, dyslipidaemia and primary valvular heart disease (moderate mitral insufficiency due to posterior leaflet prolapse and moderate aortic insufficiency), presented to the emergency department with a 1-week history of anorexia, low back and abdominal pain, shivering episodes, progressive exertional dyspnoea, bilateral lower extremity oedema and decreased urine output. On admission, she was apyretic (tympanic temperature 37.2°C), hypertensive (162/79 mmHg) and normocardic (69 bpm). On auscultation, a grade II/VI aortic diastolic murmur and a grade II/VI mitral systolic murmur radiating to the left edge of the sternum were identified. Pulmonary crackles were also noted. Blood analysis revealed anaemia (haemoglobin 7.2 g/dl), elevated systemic inflammatory markers (leucocytosis 11,100/µl, neutrophilia 83.3%; CRP 110 mg/l), raised NT-proBNP (>175,000 pg/ml), and a non-obstructive oliguric acute kidney injury (AKI) (creatinine 3.6 mg/dl, estimated glomerular filtration rate 11.6 ml/min/1.73 m2 CKD-EPI, AKIN 3), with metabolic acidosis. Leucoerythrocyturia was also identified. Thoracic radiography showed pulmonary oedema. Thoracoabdominopelvic computed tomography documented colonic diverticulosis, with no embolic or neoplastic lesions. Blood cultures identified Streptococcus gallolyticus subsp. pasteurianus. Penicillin G was administered according to the antibiogram. Transthoracic echocardiography showed vegetations on the aortic (AV) and mitral valves (MV).
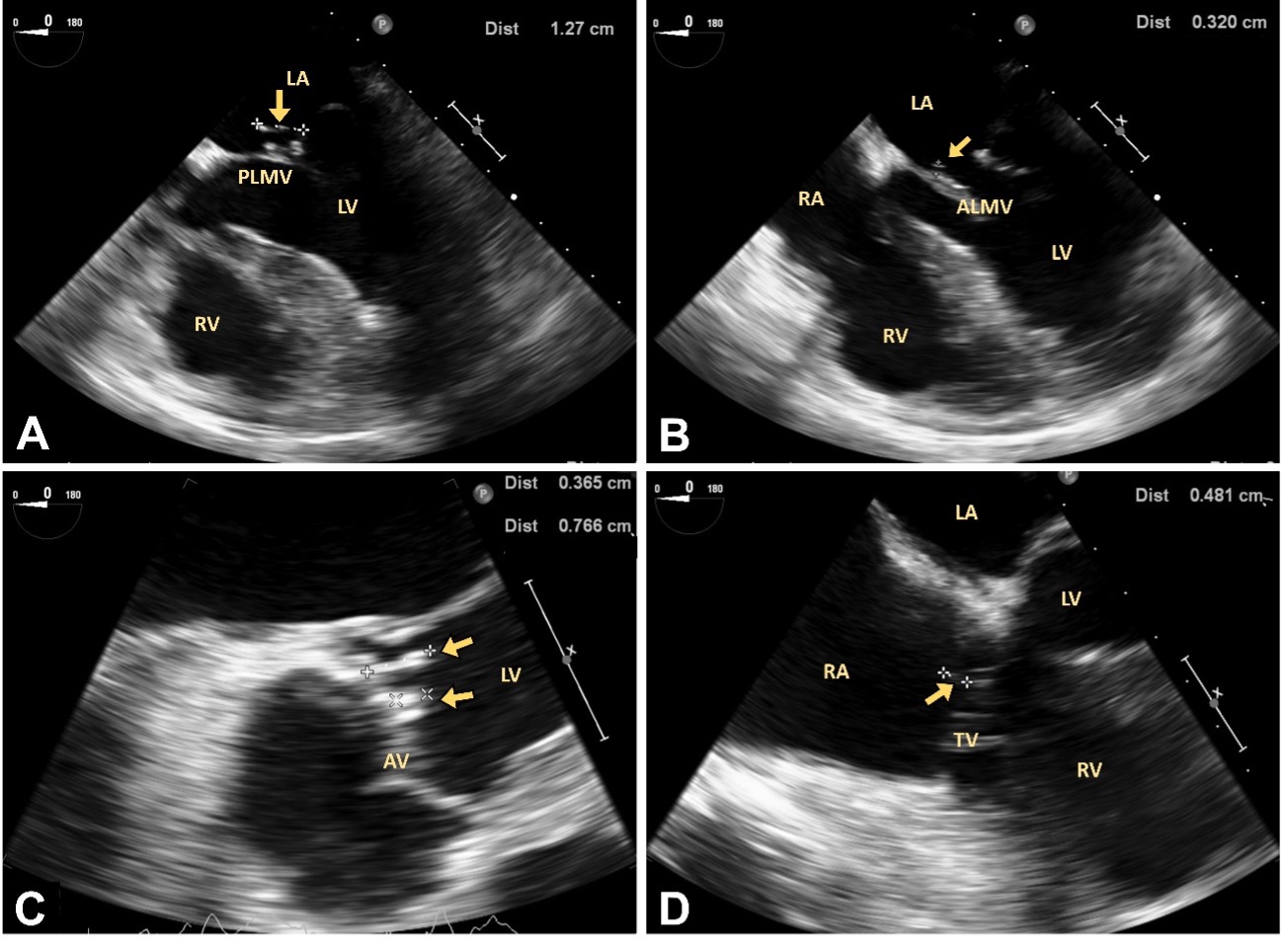
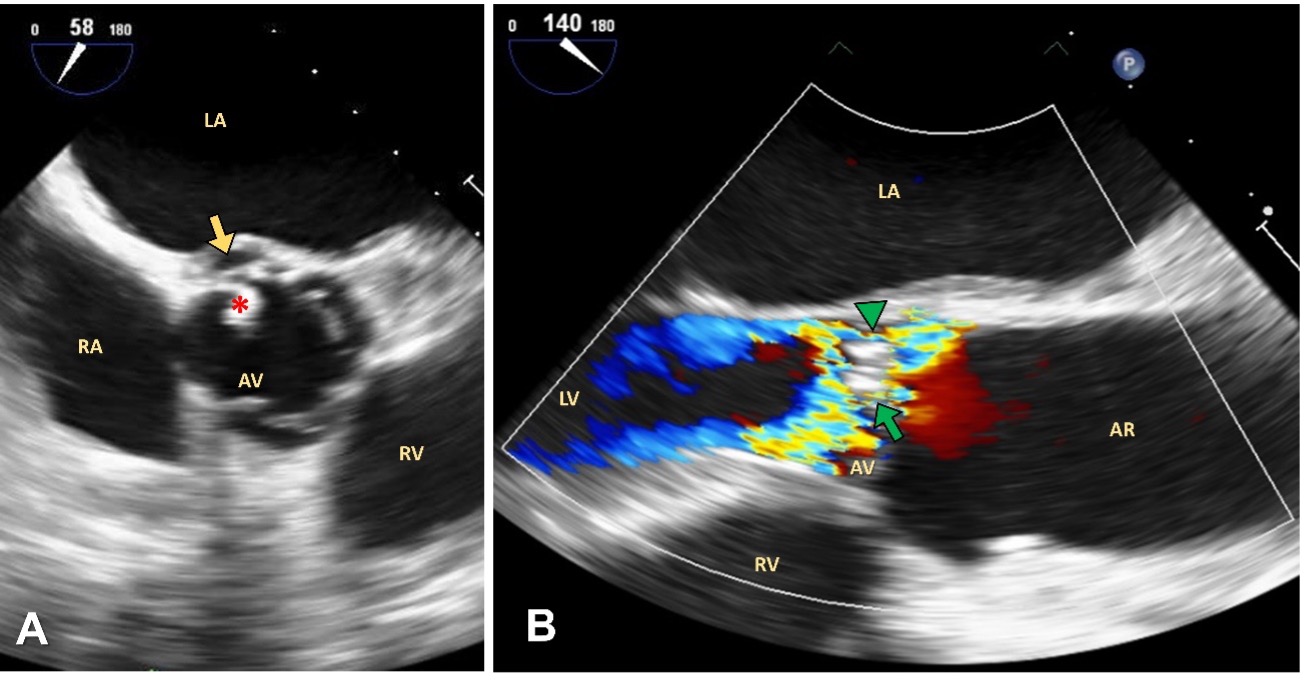
Transoesophageal echocardiography also revealed: two vegetations on the MV, one on each leaflet (Fig. 1A,B); two vegetation on the AV (Fig. 1C); one vegetation on the tricuspid valve (Fig. 1D); an abscess of the aorto-mitral curtain (Fig. 2A), and perforation of the non-coronary cusp, causing severe aortic insufficiency (Fig. 2B).
Figure 1 .Transoesophageal echocardiography showing native triple-valve endocarditis (yellow arrows indicate vegetations).
(A) Mid-oesophageal four-chamber view at 0° depicting vegetation on the atrial face of the posterior leaflet of the mitral valve (12.7 mm).
(B) Mid-oesophageal four-chamber view at 0° showing vegetation on the atrial face of the anterior leaflet of the mitral valve (3.2 mm).
(C) Mid-oesophageal five-chamber view at 0° showing two vegetations (3.7 mm and 7.7 mm) on the ventricular face of the non-coronary cusp of the aortic valve.
(D) Mid-oesophageal four-chamber view at 0° depicting vegetation on the atrial face of the septal leaflet of the tricuspid valve (4.8 mm).
ALMV, anterior leaflet of the mitral valve; AV, aortic valve; LA, left atrium; LV, left ventricle; PLMV, posterior leaflet of the mitral valve; RA, right atrium; RV, right ventricle; TV, tricuspid valve
Figure 2. Transoesophageal echocardiography showing local complications of infective endocarditis.
(A) Mid-oesophageal aortic valve short axis view at 58° showing aorto-mitral curtain abscess (yellow arrow) and aortic valvulitis (*).
(B) Mid-oesophageal aortic valve long axis view at 140° depicting two regurgitation jets, one central (green arrow) and other eccentric (green arrowhead), secondary to perforation of the non-coronary cup. AR, aortic root;
AV, aortic valve; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle
Biventricular function was preserved and no shunts were observed. Thus, the diagnosis of native triple-valve endocarditis due to S. gallolyticus was made. Because of perivalvular infection, acute heart failure (AHF) due to valvular dysfunction secondary to perforation of the non-coronary cusp, and rapid deterioration of renal function, the patient was transferred to the Cardiothoracic Surgery Department for emergent surgery. A tricuspid valvuloplasty and MV and AV replacement were performed. Although no complications occured during surgery, the patient never recovered consciousness and eventually died.
DISCUSSION
About 15% of endocarditis cases are multivalvular and most involve the AV and MV [1]. Native triple-valve involvement is extremely rare. In a recent review, only 15 cases of triple-valve endocarditis were identified [2]. These cases are usually associated with intracardiac devices, use of injectable drugs or congenital heart disease with intracardiac shunt [1, 2]. We have described an unusual case of triple-valve endocarditis with none of these predisposing conditions. Given the previous valvular anomalies in our patient, the left heart valves were probably the first affected.
S. gallolyticus has been associated with infective endocarditis with extensive local infection and multivalvular involvement [1, 3], so we speculate that it may also have played an important role in this presentation. To our knowledge, this is the first report of native triple-valve endocarditis caused exclusively by S. gallolyticus, involving the aortic, mitral and tricuspid valves. S. gallolyticus has also been associated with colonic and hepatobiliary pathology [3, 4]. Our patient had diverticulosis, a benign condition that predisposes to S. gallolyticus bacteraemia[4]. Unfortunately additional study was not possible as the patient died; however, gastrointestinal endoscopy is important as bacteraemia frequently precedes gastrointestinal symptoms, allowing early diagnosis [3, 4].
It is unclear whether multivalvular involvement is an independent prognostic factor affecting survival [1, 2, 5, 6]. However, it does seem to more frequently require surgery [1, 5]. As noticed in this case, multivalvular involvement may be associated with a higher risk of perivalvular suppurative complications and AHF, often necessitating early surgery [1, 2, 6]. Early intervention, particularly before the development of suppurative complications, is important for therapeutic success [2, 5]. The presence of abscess, reflecting advanced local disease, confers greater technical complexity, being a predictor of post-intervention mortality [1, 5]. AKI and AHF have also been identified as independent predictors of hospital mortality [1, 5]. Our patient presented all these conditions, resulting in a poor prognosis and a therapeutic challenge.
In conclusion, native triple-valve endocarditis is a rare entity, especially in the absence of predisposing conditions. We hypothesized in this case that S. gallolyticus may have played an important role. Early surgery is often required, and timely recognition and treatment, before complications develop, may be decisive for prognosis. However, since only anecdotal cases have been published, information regarding the main characteristics, optimal management and prognosis of triple-valve endocarditis is lacking, highlighting the importance of reporting this condition.