ABSTRACT
Ovarian vein thrombosis (OVT) is a relatively rare, but serious disease more commonly seen in puerperal patients. In the postpartum period, there is an unequal incidence of OVT in women with vaginal delivery (0.18%) and caesarean section (2.0%).OVT is usually associated with other conditions like pelvic inflammatory disease, malignant tumours, sepsis, enteritis, and recent pelvic or abdominal surgery. The incidence of idiopathic OVT is extremely rare and only a few cases have been reported to date in healthy patients with unknown aetiology. Patients with OVT present with abdominal pain, nausea, vomiting, fever or abdominal mass. Complications of OVT include pulmonary embolism, ovarian infarction, sepsis and death. CT scanning of the abdomen provides reliable evidence for the diagnosis of idiopathic OVT. Thrombus in most patients with idiopathic OVT is located in the right ovarian vein. This may be due to the longer length of the right ovarian vein, right shift of the uterus and relative insufficiency of the right ovarian vein valve. Treatment of OVT includes systemic anticoagulation which will achieve resolution of symptoms and prevent life-threatening complications. Our case report documents a non-puerperal patient who underwent hysterectomy a year before presenting to the ED with complaints of diarrhoea and found to have OVT on a CT scan. Our case brings attention to the fact that OVT can occur outside the puerperium and might present as a rare complication of minimally invasive surgeries for endometrial cancer. Furthermore, we posit that OVT in the non-puerperal patient may be a separate clinical entity.
LEARNING POINTS
- Ovarian vein thrombosis (OVT) can occur outside the puerperium and might present as a rare complication of minimally invasive surgeries.
- OVT should be included in the differential diagnosis of a non-puerperal postoperative woman presenting with vague abdominal symptoms.
- Duration of anti-coagulation varies from case to case. More research is needed to determine its exact duration.
KEYWORDS
Ovarian vein thrombosis, anticoagulation, gynaecological surgery
CASE DESCRIPTION
A 58-year-old woman presented with a 24-hour history of epigastric pain, sharp in onset, and non-radiating. She also had associated non-bloody, watery diarrhoea that started 24 hours after eating spicy ramen. She denied abdominal distension, nausea, vomiting, fever, chills, vaginal discharge, polyuria, dysuria and haematuria. She had undergone a robot-assisted hysterectomy, sentinel lymph node mapping and excision in August 2020 for endometrial cancer. The patient had not received any chemoradiation. Of note, the patient had received the Pfizer COVID vaccine booster 8 days before she presented to us with her current symptoms. She notably had a history of hyperlipidaemia for which she was taking Lipitor 10 mg once daily. She had no previous history of blood clots and no family history of thromboembolic or bleeding disorders.
The patient was normotensive and afebrile at presentation in the emergency department. Abdominal examination was unremarkable with no tenderness, no guarding or rigidity, no palpable liver edge, and no fluid waves. A pelvic exam revealed normal external genitalia, with surgically absent cervix and uterus, and no adnexal masses were palpable. The patient’s urine pregnancy test was negative. Her reverse transcription-polymerase chain reaction (RT-PCR) for SARS Coronavirus 2 was negative. The initial laboratory values showed WBC 4.2×103/µl, Hb 12.5 g/dl, platelets 210×103/µl, SGOT 29 U/l, SGPT 34 U/l and lipase 22 U/l.
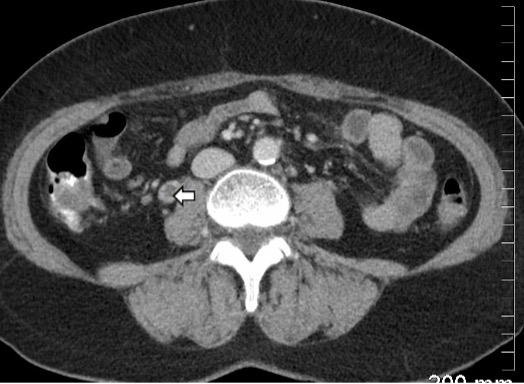
CT imaging of her abdomen and pelvis with intravenous contrast revealed that the right ovarian vein was dilated, measuring up to 12 mm with a moderate central filling defect suggestive of right ovarian vein thrombosis (OVT) (Figs. 1 and 2). No other significant findings were noted on CT scan.
Figure 1. Axial contrast-enhanced CT image demonstrates a filling defect suggestive of thrombus (dark area with an arrow) in the right ovarian vein with contrast outlining the thrombus
Figure 2. Coronal reformatted image shows the contrast outlining the thrombus (dark area, arrows) in an enlarged right ovarian vein
The patient was treated with apixaban 10 mg twice daily for 7 days followed by 5 mg twice daily. A CT scan done after 3 months of therapy showed a significant reduction in the size of the thrombus (Fig. 3). She reported significant improvement in her symptoms after 1 month and continues to take apixaban, with the plan to discontinue treatment after 6 months with repeat imaging.
Figure 3. Coronal MIP (maximum intensity projection) image showing the residual thrombus (arrows) in the distal right ovarian vein
DISCUSSION
This case of OVT raises multiple topics for discussion including the fact that OVT can occur outside the puerperium and in patients who have undergone minimally invasive surgeries. OVT is a rare venous thromboembolic disease of puerperium that affects 0.05–0.18% of postpartum women [1]. Many other conditions might be associated with OVT, such as malignancies, pelvic inflammatory diseases, sepsis and pelvic surgeries. Rarely, it can be idiopathic and occur spontaneously without any underlying risk factors or hypercoagulable disorders [2,3].
Several physiological and anatomic factors predispose women to right ovarian thrombosis. Studies have shown that 80% of cases affect the right ovarian vein, while the left ovarian vein and both ovarian veins are involved in 6% and 14% of cases, respectively. The increased involvement of the right ovarian vein may be explained by compression of the inferior vena cava (IVC) and right ovarian vein due to dextrorotation of the uterus during pregnancy. Other contributory factors are antegrade flow of blood in the right ovarian vein favouring bacterial infection, in contrast to retrograde blood flow in the left ovarian vein. The right ovarian vein also has multiple incompetent valves making it more prone to thrombosis [4].
OVT has a variable presentation. Many patients will have non-specific symptoms including fever, malaise, nausea, vomiting, abdominal pain, shortness of breath or palpable abdominal mass.
Contrast-enhanced CT of abdomen and pelvis is considered the diagnostic modality of choice for OVT [5]. Other imaging modalities include magnetic resonance angiography (MRA) and colour Doppler ultrasound. MRA offers several advantages over CT in the diagnosis of OVT as it avoids ionizing radiation, has sensitivity and specificity approaching 100% compared to CT with a sensitivity of 77.8% and specificity of 62.5%, and avoids intravenous contrast administration secondary to the use of diffusion weighted imaging [5,6]. Ultrasound with Doppler may be used for follow-up of OVT patients after treatment is initiated; its sensitivity in the diagnosis of OVT is 52% and is poorer than CT or MRA [7,8].
Complications of OVT include pulmonary embolism which can be seen in 3–33% of the cases with a mortality of 4.0%. OVT can also extend to renal veins and the IVC leading to ovarian infarction, ureter obstruction or kidney rupture.
The mainstay of management is anticoagulation. Resolution of OVT has been documented after 7–14 days of anticoagulation therapy [9]. Other studies have reported that OVT may not resolve with short anticoagulation therapy and 3–6 months of anticoagulation is indicated until radiologically confirmed resolution of the thrombus. Direct oral anticoagulants like apixaban and rivaroxaban have been reported to be efficacious for the treatment of OVT [10,11]. Anticoagulation is also indicated if the clot extends to the IVC [12].
CONCLUSION
OVT should be included in the differential diagnosis of postoperative non-puerperal woman presenting with vague abdominal symptoms. Complications include pulmonary embolism, sepsis and thrombus extension. Management includes anticoagulation therapy to avoid complications. Furthermore, given that non-puerperal OVT is a rare diagnosis, further study is indicated to establish if it is a different clinical entity from puerperal OVT.