ABSTRACT
A young man was treated in hospital for sepsis, disseminated intravascular coagulation and multi-organ failure. He was a regular intranasal cocaine user up to 1 day prior to symptom onset. Clinical examination revealed extensive retiform purpura affecting both his lower limbs. Skin biopsy revealed widespread thrombosis in the small- and medium-sized vessels of the mid dermis and the subcutaneous fat with surrounding leucocytoclasis. There was also extensive ischaemic necrosis of the upper reticular and papillary dermis and focal ischaemic necrosis of the epidermis. These findings were in keeping with a thrombotic vasculopathy with associated cutaneous ischaemic necrosis, likely associated with levamisole-adulterated cocaine (LAC). An autoimmune screen showed extremely raised levels of anti-B2-glycoprotein IgM, IgG and anti-cardiolipin IgG antibodies, usually seen in antiphospholipid syndrome (APS). The literature describes how APS could be secondary to various underlying conditions, including LAC, and that levamisole toxicity may mimic APS and hence be missed.
LEARNING POINTS
- Levamisole is a common adulterant found in cocaine; the resultant toxicity can present with cutaneous manifestations, namely retiform purpura and skin necrosis, similar to antiphospholipid syndrome.
- Patients presenting with such features should be asked about illicit drug use, specifically cocaine, and investigated by screening urine for drugs of abuse and serum antihuman elastase antibody when possible.
KEYWORDS
Cocaine, levamisole, antiphospholipid syndrome, vasculitis, retiform purpura
CASE DESCRIPTION
A 31-year-old Caucasian man presented to hospital with a 3-day history of rapidly worsening lethargy, persistent fever, loose stools and cough. Self-medication with paracetamol and NSAIDs was ineffective. He admitted to regularly snorting cocaine up to 1 day before symptom onset. At 10 years of age, the patient had been anticoagulated for a right lower limb deep vein thrombosis and bilateral pulmonary emboli. He was also diagnosed with liver cirrhosis of unknown aetiology at 18 years of age. Aspirin 75 mg daily was the only regular treatment.
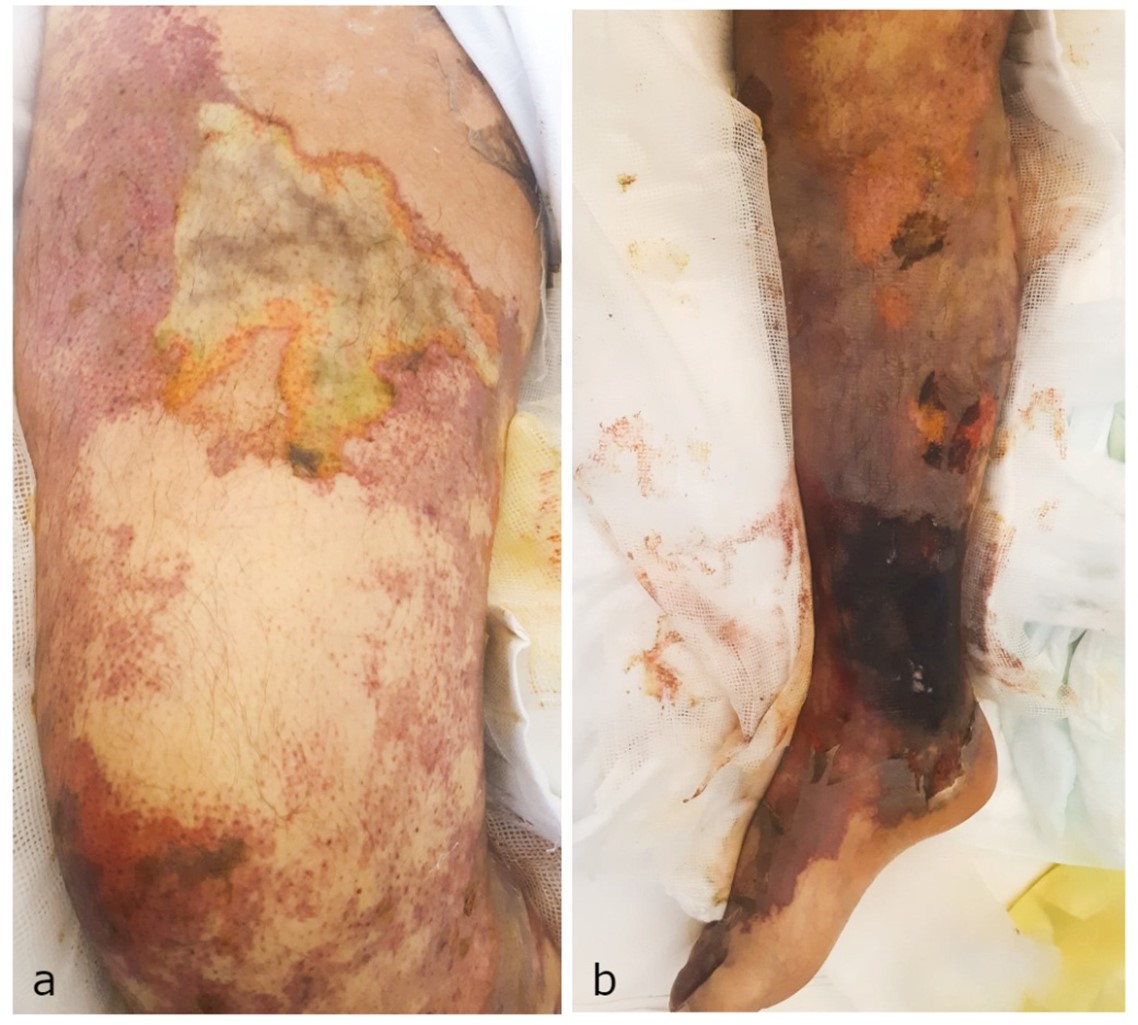
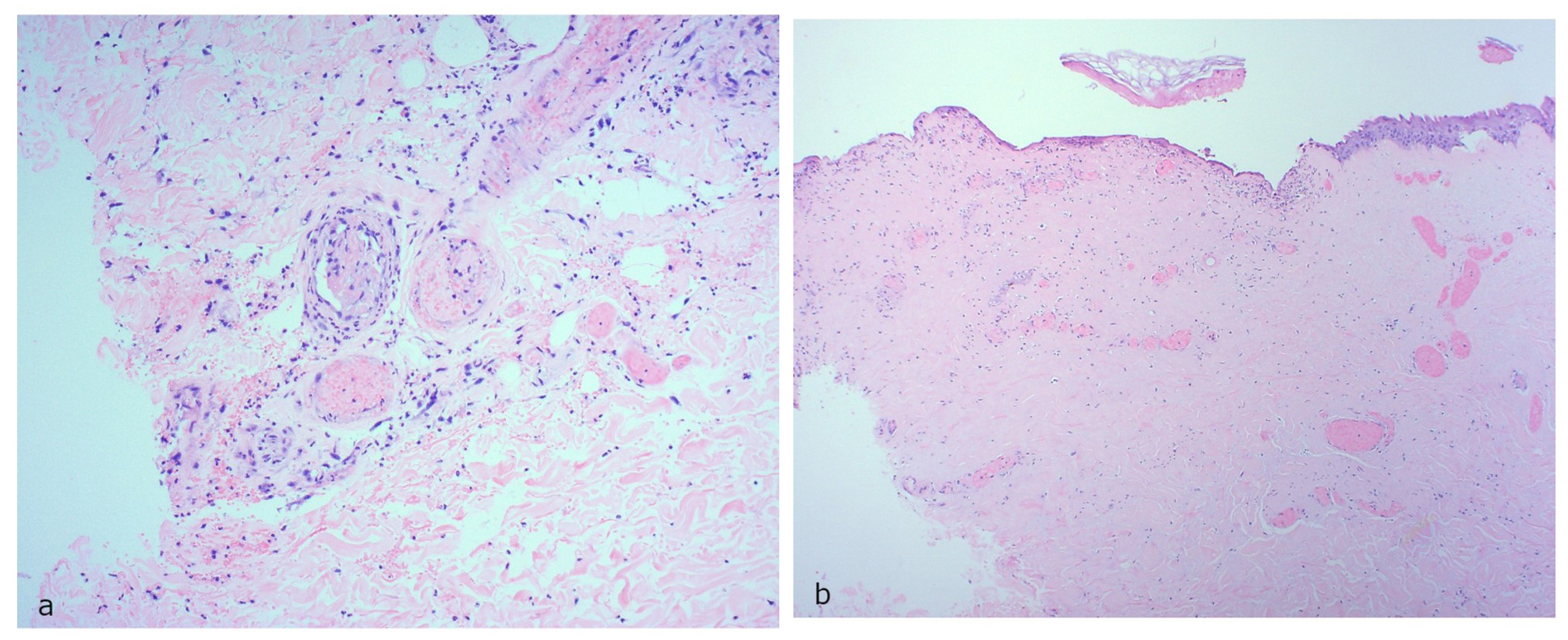
On admission, widespread livedoid purpura with epidermal peeling, areas of necrosis and erosions were noted over both lower limbs (worse on the right) extending from the thighs to the feet. These had been developing progressively over the previous 3 weeks (Fig. 1). Dermatology was consulted 1 week into admission, and a large wedge biopsy was taken from the edge of an eroded area on the right thigh. Histological examination revealed widespread thrombosis in the small- and medium-sized vessels of the mid dermis and the subcutaneous fat with surrounding leucocytoclasis (Fig. 2a). There was also extensive ischaemic necrosis of the upper reticular and papillary dermis and focal ischaemic necrosis of the epidermis. These findings were in keeping with a thrombotic vasculopathy with associated cutaneous ischaemic necrosis (Fig. 2b).
Figure 1. Widespread livedoid purpura with epidermal peeling, areas of necrosis and erosions over the right lower limb extending from the thigh (a) to the foot (b)
Figure 2. (a) Intraluminal thrombi identified in small- and medium-sized vessels in the dermis (haematoxylin and eosin (H&E) stain ×200). (b) Extensive ischaemic necrosis of the upper reticular and papillary dermis and focal ischaemic necrosis of the epidermis (H&E stain ×40)
A urine sample for toxicology taken on admission was positive for cocaine. Blood tests revealed acute kidney injury with hyperkalaemia, decompensated liver disease and lactic acidosis. Inflammatory markers were raised and leucocytosis and thrombocytopaenia were noted.
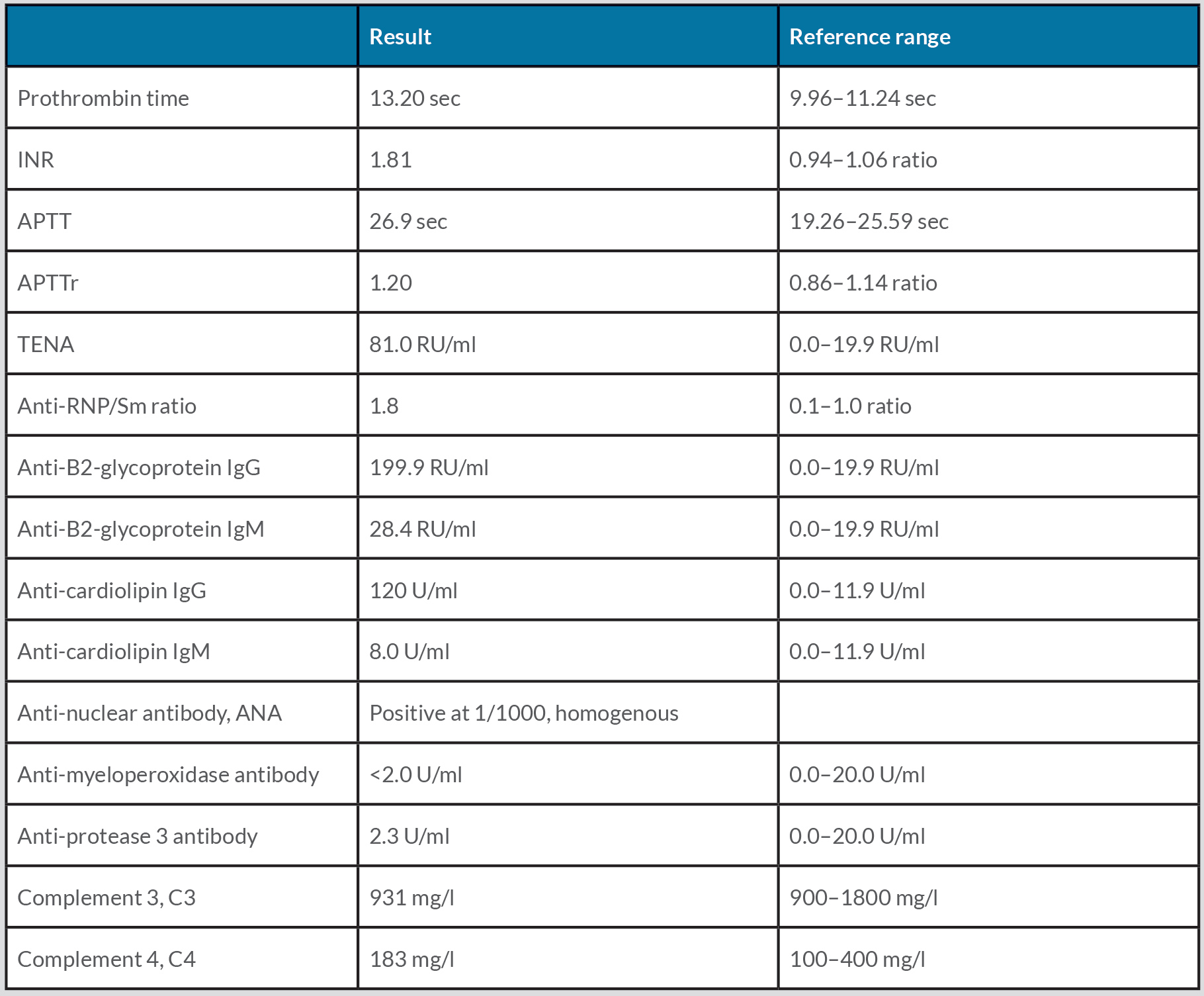
The coagulation profile was mildly elevated. An autoimmune screen was positive for total extractable nuclear antigen, ANA (homogenous), anti-RNP/Sm, anti-B2-glycoprotein immunoglobulins and anti-cardiolipin IgG antibodies (Table 1). A lupus inhibitor profile was also positive. ANCA was negative. It was not feasible to screen for protein C, protein S, antithrombin III and factor V Leiden profiles as the patient was acutely unwell.
These findings were strongly suggestive of LAC-associated retiform purpura in the context of underlying antiphospholipid syndrome (APS).
The patient was treated with intravenous antibiotics for sepsis and during his stay required admission to the Intensive Care Unit in view of disseminated intravascular coagulation in the context of multi-organ failure. The necrotic wounds in the lower limb were treated with chlorhexidine-containing paraffin dressings; however, the ulceration became progressively more extensive with overlying gangrene necessitating a right above-knee amputation. The patient also developed complications related to cirrhosis and portal hypertension (upper gastrointestinal bleeding, rectal bleeding, portal enteropathy, hepatorenal syndrome, encephalopathy), coagulopathy (bilateral pulmonary emboli, splenic infarction) and the hospital stay (bilateral pneumonia). Anticoagulation was therefore not deemed safe in this context. Despite treatment, the patient died 9 weeks after admission to hospital.
DISCUSSION
LAC-associated retiform purpura is an emerging phenomenon of public concern first reported in 2010 [1]. Levamisole is a veterinary anthelmintic agent which had historically been used as an immunomodulatory agent in oncology and paediatrics, but its use was discontinued in the late 90’s mainly due to a significant risk of agranulocytosis and retiform purpura. These manifestations have since been reported in patients who are known cocaine users, and levamisole seems to be the main potentiating agent. Apart from being a cheaper cocaine cutting agent, it is thought that levamisole can prolong cocaine-induced euphoria via potentiation of the nicotinic acetylcholinergic pathway in the central nervous system and through the metabolism of levamisole to aminorex, which is an amphetamine that acts as an indirect serotonin agonist [2].
LAC-associated retiform purpura commonly affects the face, ears and abdomen [3, 4, 5], however, presentation at other sites, such as on the thighs, has also been reported [3, 5]. Histological features may vary but typically exhibit one or more of leucocytoclastic vasculitis, vasculopathy, thrombotic microangiopathy, panniculitis and/or necrosis [6].
Typical findings on laboratory blood testing include neutropenia, leucopenia and agranulocytosis. An autoimmune screen may be positive for one or more of lupus anticoagulant, anti-ds DNA, ANA, ANCA and antiphospholipid antibodies (aPL). Around 90% of reported cases of LAC-associated retiform purpura in the literature are positive for ANCA, with proteinase 3 (PR3) positivity being more common than myeloperoxidase (MPO) positivity. Our case is unusual due to its lupus anticoagulant, aPL and ANA positivity, but ANCA negativity. ANA and lupus anticoagulant positivity are reported in around 50% of cases in the literature [2]. Antiphospholipid antibody positivity has also been reported [5]. Complement testing may show normal or mild hypocomplementaemia. Antihuman elastase antibody is specific and sensitive for levamisole-induced vasculitis [6], however this test is not easily accessible and was not available in our case.
Retiform purpura in the context of APS is an intriguing feature which has been documented many times in the literature. APS can in fact be secondary to LAC and present with positive antiphospholipid antibodies and thrombosis on histology. We speculate that our patient already had a genetic susceptibility for coagulopathies and LAC acted as a trigger for his presentation [4, 5].
One possible mechanism behind cocaine-associated thrombotic vasculopathy and vasculitis proposed by Magro and Wang is that cocaine and its metabolites may induce intercellular adhesion molecule-1 (ICAM-1) and C5b-9 deposition, respectively, leading to a cascade of events ultimately causing thrombotic microangiopathy and inflammatory vasculitis. Antiphospholipid antibodies and ANCA possibly form a part of this cascade which promotes a proapoptotic microenvironment [1]. This possibly explains why levamisole toxicity can mimic APS in clinical features, histological changes and immunological profile.
Failure to enquire about illicit drug use could lead to the diagnosis of LAC-induced vasculitis being missed. This is especially the case because urine drug toxicology screening may only detect cocaine 48–72 hours after use and levamisole is even harder to detect given its short half-life of 5.6 hours [6].
CONCLUSION
LAC-associated retiform purpura is a potentially serious complication of cocaine use which can lead to sepsis and death. It is therefore important to differentiate it from other causes of retiform purpura so that cocaine use is stopped and appropriate supportive care is provided.