ABSTRACT
Introduction: Deep neck abscess in adults may occur as a result of local trauma, foreign body inoculation or immunosuppression.
Method: We describe a case of deep neck abscess that developed after recent hospitalization and intubation for chronic obstructive pulmonary disease (COPD) exacerbation.
Discussion: The incidence of deep neck abscesses has dramatically reduced due to the use of antibiotics. However, if present, they need prompt surgical drainage due to their proximity to the nearby vasculature of the neck.
Conclusion: This case highlights the need for physician awareness of the clinical presentation of the unique complications of deep neck abscess developing after hospitalization.
LEARNING POINTS
- Recent intubation or the introduction of a foreign body into the airway should be considered as possible causes of deep neck abscess infection.
- The diagnosis may be suggested by a CT scan.
- Incision and drainage may be required for the treatment of deep neck space infection.
KEYWORDS
Deep neck space, parapharyngeal abscess, methicillin-resistant Staphylococcus aureus, MRSA, intubation
INTRODUCTION
Infections that affect the parapharyngeal space may be secondary to penetrating trauma or foreign body ingestion associated with orotracheal intubation, laryngoscopy, or passage of a nasogastric tube. Here, we present the case of a 47-year-old man who developed a right-sided deep neck abscess after recent hospitalization and intubation. This case is being reported to increase awareness of such rare complications after intubation and the importance of prompt diagnosis and surgical drainage to improve outcome.
CASE DESCRIPTION
A 47-year-old man with a medical history of hypertension, chronic obstructive pulmonary disease (COPD) and gastric band surgery presented to the emergency department (ED) with the chief complaints of chest pain and difficulty swallowing for the past 2 days. The chest pain was sudden in onset, continuous, reproducible with touch, radiating to the right side of the neck, associated with nausea and non-bloody vomiting, and without any aggravating or relieving factors. The patient also reported difficulty swallowing both solids and liquids for the past 3 days along with subjective fever and chills. He denied any palpitations, cough, abdominal pain, change in bowel movements or any similar symptoms in the past. Review of systems was otherwise negative. He was a former smoker with occasional marijuana use but denied any intravenous drug abuse. The patient had been admitted to another hospital a week earlier for COPD exacerbation that required intubation. He had been extubated and discharged on steroids.
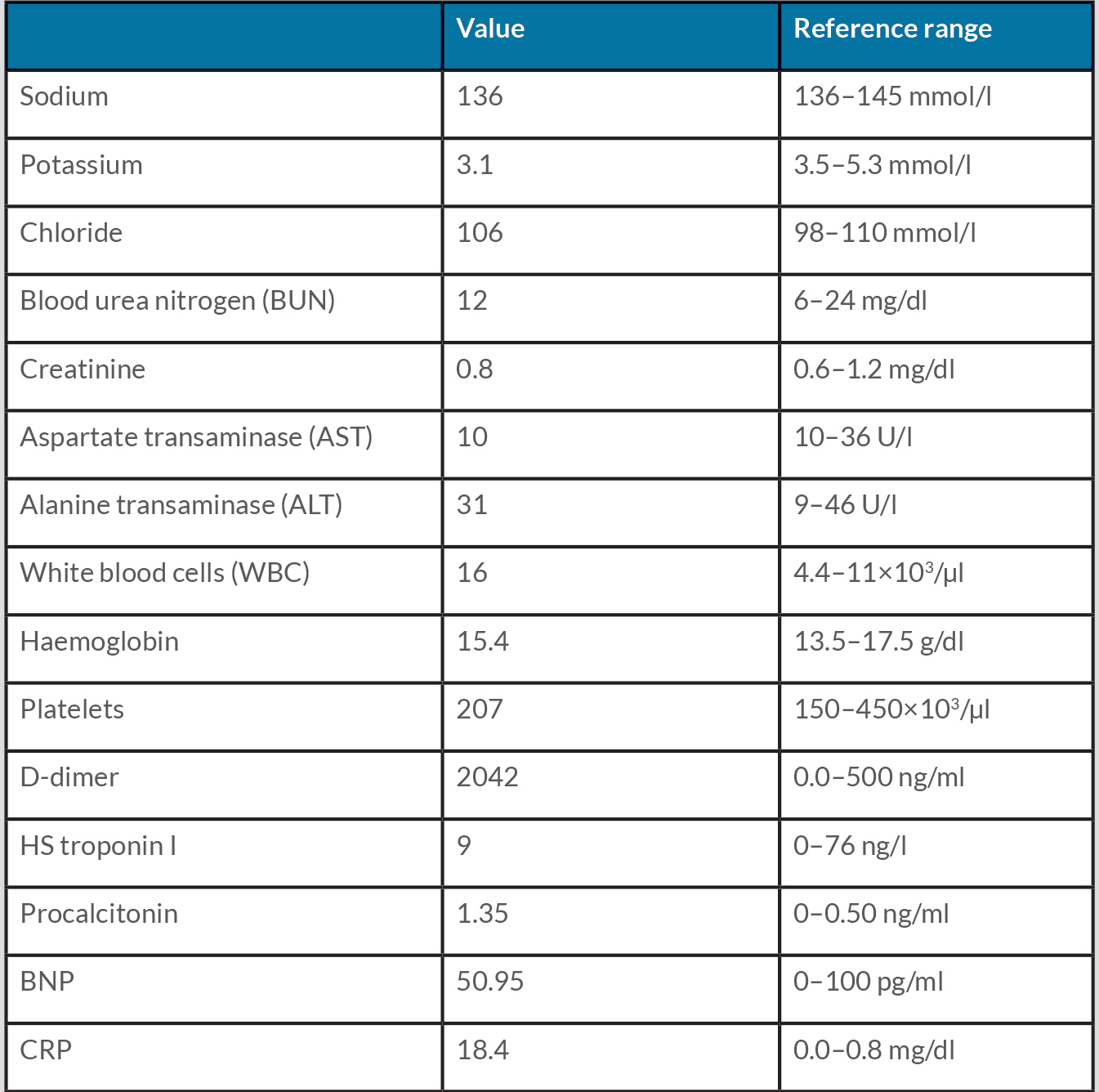
On admission, his temperature was 37.2°C, pulse 94/min, blood pressure 130/79 mmHg, oxygen saturation on room air 98%, and respiratory rate 25 breaths per minute (BPM). On physical examination, the patient was in acute distress due to chest pain. Respiratory examination was positive for bilateral diffuse crackles. Heart sounds were normal without any murmurs. There was tenderness on palpation of the right upper sternal and suprasternal region and right infraclavicular region. No erythema, warmth or swelling was noted. The remainder of the physical examination was unremarkable. Initial laboratory examination was significant for leucocytosis. His C-reactive protein (CRP), D-dimer and procalcitonin levels were elevated. Initial laboratory findings are shown in Table 1.
Chest x-ray was unremarkable. Electrocardiography (EKG) showed sinus rhythm with no ST-T wave abnormalities. Echocardiography showed an ejection fraction of 65–70%. Computed tomography angiography (CTA) of the chest showed a patulous oesophagus with hyperdense material in the distal oesophagus. Computed tomography (CT) of the neck with contrast showed soft tissue swelling and oedema along the right side of the lower neck near the sternocleidomastoid and the right sternoclavicular articulation. Ultrasound of the soft tissue of the neck showed an abnormal heterogeneous area approximately 3.5 cm in size compatible with myositis at the base of the neck without evidence of abscess. Magnetic resonance imaging (MRI) of the neck without contrast showed a 5×3×5 cm area of myositis involving the musculature at the base of the right neck with no associated synovitis of the sternoclavicular joint. The blood cultures (2 sets and 4/4 bottles) came back positive for coagulase-positive gram-positive cocci (GPC) in clusters and the patient was started on vancomycin and cefazolin. Cefazolin was discontinued after the bacterium was identified as methicillin-resistant Staphylococcus aureus (MRSA).
Transthoracic echocardiography (TTE) was performed to rule out infective endocarditis and was negative for vegetations. Transesophageal echocardiography (TEE) was not done because of migration of the gastric band. Due to persistent bacteraemia with no apparent source, antibiotics were switched to daptomycin and ceftaroline. The patient was also complaining of worsening neck pain and a repeat CT scan of the neck with contrast showed a right-sided supraclavicular neck abscess which was displacing the trachea and the thyroid with compression of the jugular vein as shown in Fig. 1. Incision and drainage (I&D) were done, and culture grew MRSA. Repeat blood cultures after I&D were negative (first negative blood culture after the source control). The patient improved clinically and was discharged on daptomycin IV for 2 weeks and then de-escalated to oral linezolid as an outpatient for 6 weeks in total from the first negative blood culture.
Figure 1. Right-sided supraclavicular neck abscess (red arrow) displacing the trachea and the thyroid with compression of the jugular vein
DISCUSSION
Deep neck space infections (DNSI) refer to an infection in the fascial planes of the neck which either results in cellulitis or abscess formation[1]. The deep spaces are classified into three categories based on their relationship to the hyoid bone. The first category involves the space above the hyoid bone such as the peritonsillar, parapharyngeal, submandibular and parotid spaces. The second category involves the entire circumference of the neck including the retropharyngeal, prevertebral and carotid spaces, while the third category includes the pretracheal visceral space below the hyoid bone [2]. Infections of the deep neck are difficult to localize and diagnose since the affected tissue may be deep and impossible to palpate or visualize [3]. Common sources of DNSI include malignancies, foreign bodies, tonsillar infections and dental infections [2]. DNSI are usually polymicrobial in nature. A study conducted by Parischar et al. showed that Streptococcus was the most commonly cultured organism [4].
The clinical manifestations are variable and can present as fever, fatigue, swelling, odynophagia, otalgia or dyspnoea [5]. The non-specific symptoms might lead to a delay in diagnosis which may result in a fatal outcome. Our patient spontaneously developed a supraclavicular abscess after recent hospitalization, with cultures positive for MRSA bacteraemia. Intubation could introduce MRSA bacteria, which later leads to a supraclavicular neck abscess while the patient is on high-dose steroids, and eventually results in persistent bacteraemia. MRI and CT play a pivotal role in the diagnosis of deep neck abscess. The management plan includes antibiotics, airway management and possible surgical intervention. In our patient, antibiotics and I&D relieved the symptoms.
Despite the extensive use of antibiotics, these infections can be potentially life threatening, with severe complications if left untreated. Commonly reported complications include airway obstruction, cavernous sinus thrombosis, sepsis and haematogenous spread to distant organs. Physician awareness of this pathology along with prompt diagnosis and management can prevent complications and reduce morbidity and mortality.