ABSTRACT
Prothrombin time (PT), first used in 1935, is the most commonly employed marker of coagulopathy to assess bleeding tendency. It is a screening test and measures the time in seconds to the formation of a clot after platelet-poor plasma has been mixed with a thromboplastin reagent consisting of tissue factor, lipids and calcium chloride ions. The International Normalized Ratio (INR) is a standardized number based on the PT of the patient. It is used by clinicians to measure the effectiveness of anticoagulants and to guide therapy. Drugs such as warfarin can affect the level of or the metabolism of vitamin K in the body, which can impact PT and INR levels. A supratherapeutic INR is rare in a patient not on therapy with vitamin K inhibitors and with preserved liver function. Here we describe an elderly man with a supratherapeutic INR, secondary to the use of rifampin. Antibiotic-induced coagulopathy is an extremely rare complication. To the authors' knowledge, this is a unique case of rifampin-induced coagulopathy with no other associated complications of disseminated intravascular coagulation. A literature review revealed a small number of cases of rifampicin-induced coagulopathy. A high index of suspicion and knowledge is essential for the diagnosis and management of such cases.
LEARNING POINTS
- Given the unpredictability and rarity of rifampicin-induced coagulopathy in clinical practice, clinicians should be aware of the possibility of bleeding or drug-induced thromboembolic events with antibiotics.
- Early recognition and withdrawal of the offending agent are key to the successful management of this condition.
- Clinicians should be aware of the possible side effects of administered drugs and their possible interactions.
KEYWORDS
Coagulopathy, rifampin, INR
CASE DESCRIPTION
The patient was an 88-year-old man with a medical history of hypertension and infective endocarditis from methicillin-sensitive Staphylococcus aureus (MSSA) bacteraemia, presented to the emergency room from a rehabilitation facility for evaluation of asymptomatic anaemia; a haemoglobin (Hb) of 6.3 had been noted on laboratory work-up at the facility. A review of his medications showed that he was not on warfarin or any thromboembolism prophylaxis. He had been hospitalized 2 weeks before this admission for MSSA bacteraemia and had been discharged to the rehabilitation facility on intravenous antibiotics consisting of cefazolin, gentamicin and rifampin. Hb on the day of discharge was 9.5 g/dl.
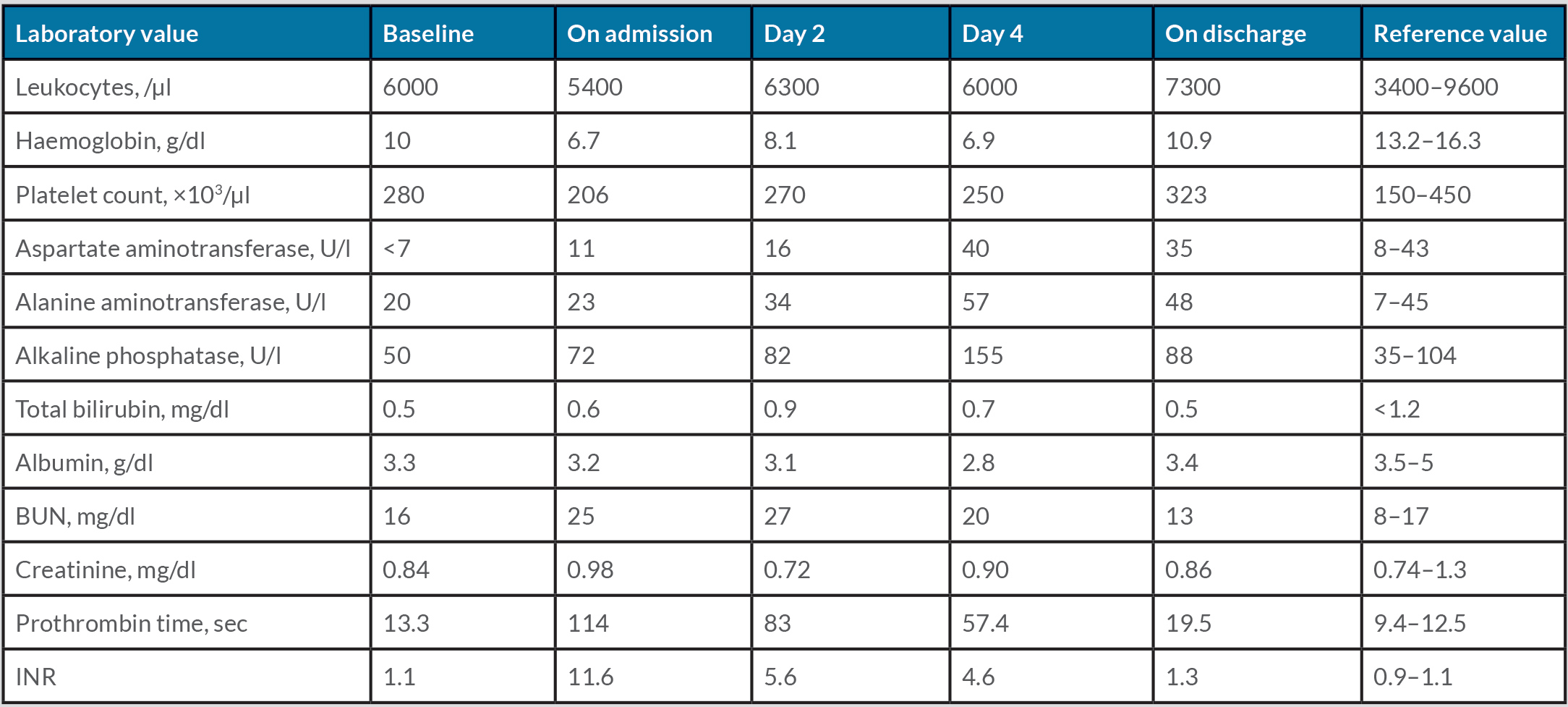
He denied any chest pain, dizziness, loss of consciousness, dark stools, blood in urine, or trauma. His vital signs were stable on admission. The physical examination revealed skin bruises on the arms bilaterally and pale palpebral conjunctiva; the rest of the examination was unremarkable. The laboratory findings on admission (Table 1) showed haemoglobin 6.3 and INR 11.6 with PT 114 and PT 73. The fibrinogen level was normal and D-dimer was slightly elevated, ruling out disseminated intravascular coagulation. The patient was given one unit of packed red blood cells (PRBC) followed by one unit of fresh frozen plasma (FFP) and some vitamin K (vitamin K levels on admission were noted to be normal). Gentamicin was discontinued due to elevated creatinine/acute kidney injury. The patient was continued on cefazolin and rifampin for MSSA bacteraemia. On day 2, Hb was 6.1, and INR 5.6 with PT 56.1 and PTT 57.4, and the patient received two more units of PRBC along with oral vitamin K. Day 3 laboratory results did not show any significant improvement in INR. Given the suspicion of coagulopathy from antibiotic use, infectious disease and haematology consultations were requested. After a multi-disciplinary discussion, it was decided to withhold rifampin, and to continue cefazolin with close monitoring. Laboratory tests were repeated the next day (day 4) and showed Hb of 9.4 g/dl, and INR 1.1 with PT 11.8 and PTT 57.4. On subsequent testing, INR remained within normal limits, which supported the suspicion that the coagulopathy had been caused by rifampin use. Given the improvement in INR after discontinuation of rifampin, cefazolin was continued through the course. A colonoscopy performed because of faecal occult blood showed caecal adenocarcinoma, which was resected via a laparoscopic right hemicolectomy. The patient’s haemoglobin and coagulation profile remained stable after surgery and he was discharged to a rehabilitation facility to complete 6 weeks of antibiotics with cefazolin and gentamicin.
Table 1. Timeline of laboratory results over the course of hospitalization
DISCUSSION
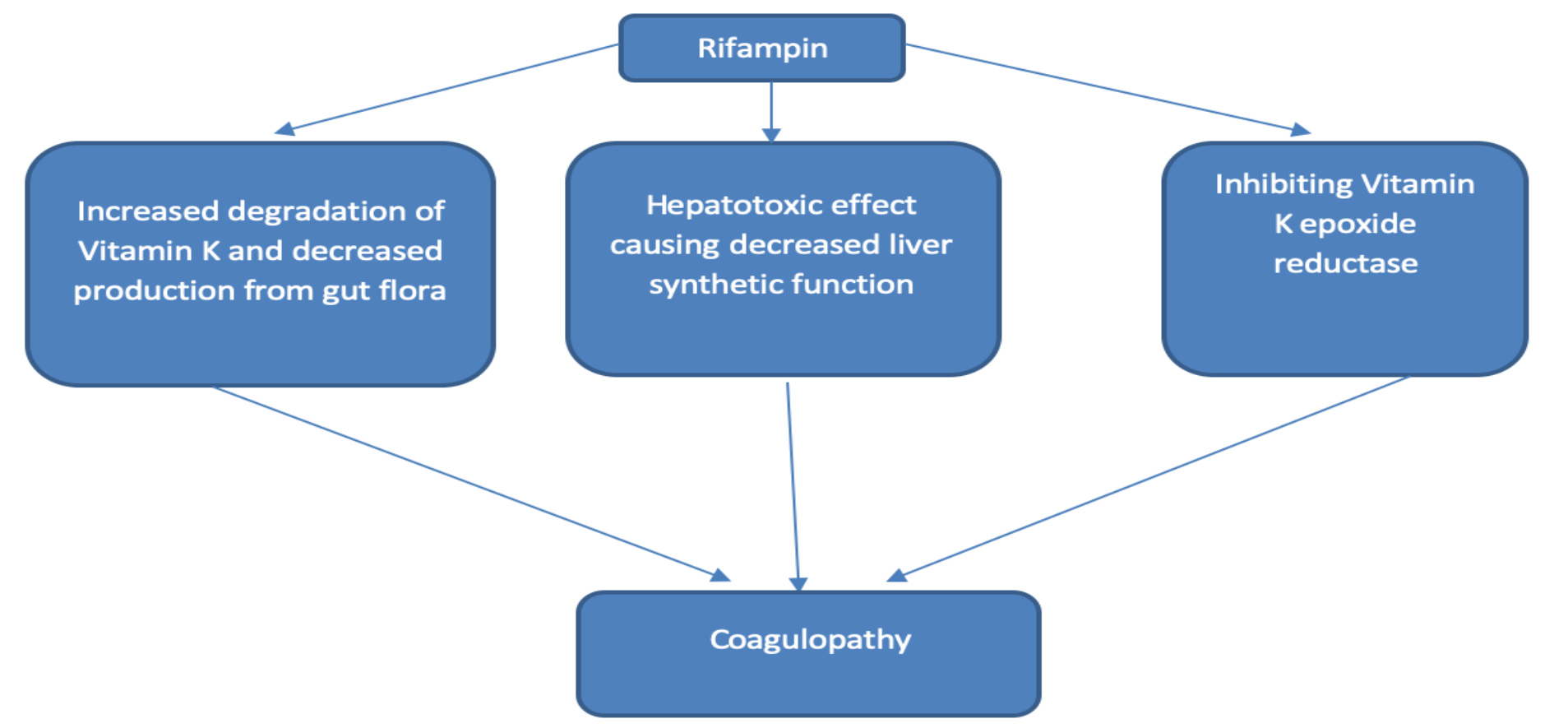
Rifampin has been implicated in causing coagulopathy by inhibiting vitamin K epoxide reductase, increasing the degradation of vitamin K by the liver due to microsomal enzyme activation, and by reducing the production of vitamin K by the gut flora [1]. Rifampin is a potent inducer of cytochrome P-450 enzymes and is also reported to cause toxic hepatitis and hypoprothrombinaemia [2]. Hypoprothrombinaemia resulting from antimicrobial therapy causing alterations in vitamin K-producing intestinal bacteria, is an extremely rare complication but is well documented for rifampicin, certain cephalosporins, and meropenem [3] (Fig. 1). This is an important consideration in patients with pre-existing vitamin K deficiency.
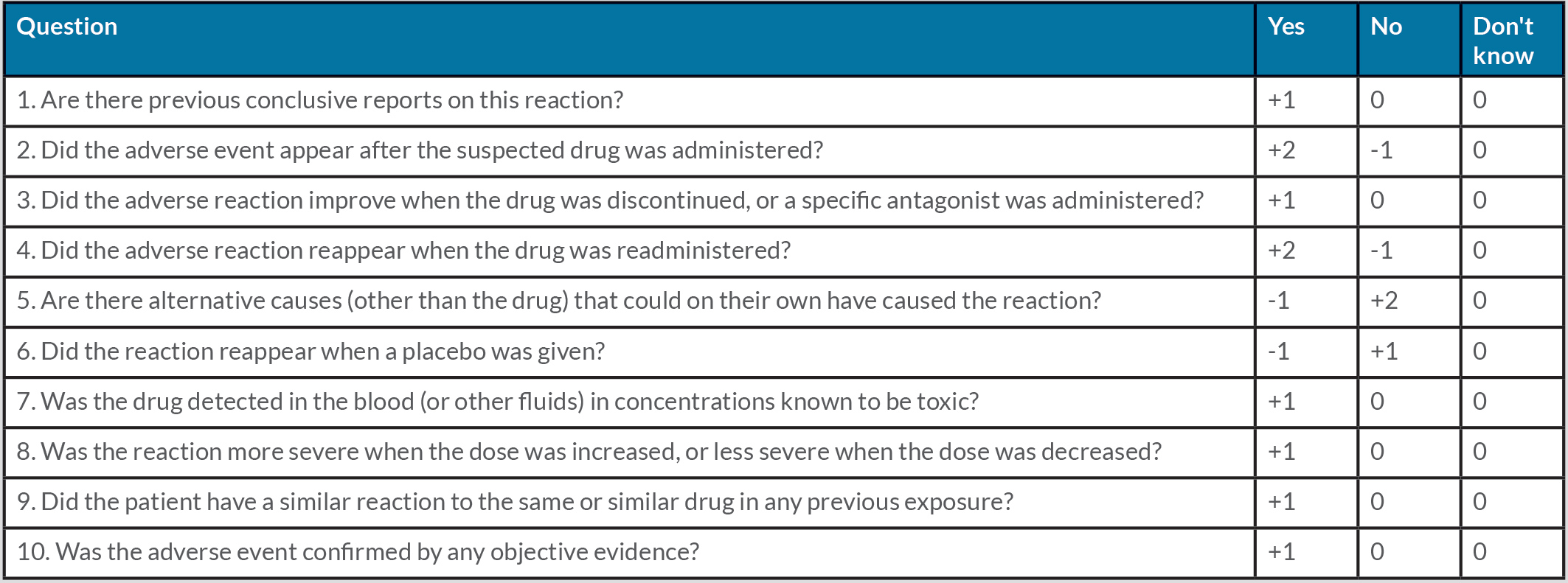
Cefazolin has been frequently implicated in coagulopathy due to the presence of a side chain that inhibits the activity of vitamin K epoxide reductase [4]. In most cases, a combination of rifampin and cefazolin has been thought to be associated with coagulopathy but in our case, the Adverse Drug Reaction Probability Scale (Naranjo) identified rifampin as the probable cause of the coagulopathy (Table 2).
Given the unpredictability and infrequent occurrence of rifampicin-induced coagulopathy in clinical practice, clinicians should be aware of the possibility of bleeding or drug-induced thromboembolic events. Early recognition and withdrawal of the offending agent are key in the successful management of this condition. Vitamin K supplementation may also have a role in correction of the coagulopathy.
Figure 1 Possible pathways of rifampin-induced coagulopathy
Table 2. Adverse Drug Reaction Probability Scale (Naranjo). The score indicates the likelihood of the drug causing the adverse drug reaction: ≥9 indicates ‘definite’, 5–8 ‘probable’, 1–4 ‘possible’, and ≤0 ‘doubtful’.