ABSTRACT
Hyponatremia is the most common electrolyte balance disorder, especially in the elderly and polymedicated population. The authors report the case of an 83-year-old man with symptomatic severe hyponatremia due to Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) related to pantoprazole. Pantoprazole was discontinued and serum sodium levels reached normal values in two months. To the authors’ knowledge, this is the second reported case of pantoprazole-related hyponatremia and, while most patients with hyponatremia related to proton pump inhibitors have mild symptoms, this patient had severe manifestations.
LEARNING POINTS
- The association between hyponatremia and proton pump inhibitors should be kept in mind when evaluating a patient with hyponatremia, especially in the elderly population.
- Hyponatremia is associated with increased risk of morbidity, which includes risk of fractures and falls, increased length of hospital stay and mortality.
- Physicians should avoid unnecessary prescriptions and always weigh the advantages and disadvantages when prescribing medications on an individual basis.
KEYWORDS
Hyponatremia; pantoprazole, proton pump inhibitors; Syndrome of Inappropriate Antidiuretic Hormone Secretion.
INTRODUCTION
Hyponatremia, defined as serum sodium concentration lower than 135 mmol/L, is the most common electrolyte balance disorder encountered in clinical practice1. It is related to a broad spectrum of conditions, clinical symptoms and poor clinical outcomes, such as increased risk of falls and fractures, cognitive impairment, osteoporosis, longer hospital stays and increased mortality2.
The prevalence of hyponatremia is known to increase in elderly and institutionalized patients, reaching an incidence as high as 30%1. Establishing its etiology is often difficult and iatrogenic hyponatremia might be an important and underdiagnosed cause, especially in elderly and frail patients taking multiple medications2.
CASE REPORT
An 83-year-old man was admitted to the Emergency Room (ER) in January 2015 with symptoms of dizziness, nausea, vomiting and anorexia, progressively evident in the previous 3 weeks. He denied other associated symptoms, such as fever, mental state alteration, cough, pain, palpitations, dysuria, pollakiuria, diarrhea, vomiting or abdominal pain.
He had a known history of arterial hypertension; type 2 diabetes; dyslipidemia; gastroesophageal reflux; and an hemorrhagic stroke (caused by the rupture of a brain aneurism at the age of 62, which resulted in sequelar mild left hemiparesis). He was medicated with carvedilol 6.25mg bid, indapamide 1.5 mg id, metformin 500 mg and vildagliptin 50 mg id, sinvastatin 40 mg and ezetimibe 10 mg id, ticlopidine 250 mg id and pantoprazole 20 mg id.
Clinical examination revealed a mild lentification and disorientation. The remainder of the physical examination showed no other relevant alterations and the neurologic exam did not show any findings other than sequelar left hemiparesis.
His blood analysis revealed a serum sodium of 116 mmol/L; serum magnesium of 1.4 mg/dL with normal serum potassium; serum osmolarity of 240 mosmol/L (280 – 300 mosmol/L); urinary osmolarity of 238 mosmol/L (300 – 900 mosmol/L) with urinary sodium of 58 mmol/L. The electrocardiogram was in sinus rhythm, with cardiac frequency of 79 bpm. A brain computerized tomography (CT) scan did not show any acute lesions.
Serum sodium was corrected with the administration of hypertonic sodium chloride (3%) and slow infusion of normotonic fluid (0.9%) and magnesium sulfate for 3 days, reaching a concentration of 133 mmol/L of serum sodium. At this point, the patient was asymptomatic and was discharged from the ER, with the indication to maintain his medication, including pantoprazole.
In February 2015, the patient was re-evaluated and was again found to be hyponatremic (serum sodium of 129 mmol/L and serum magnesium of 1.7mg/dL). At this point, he was admitted to an Internal Medicine ward for etiologic investigation. The possibility of Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) associated with pantoprazole was considered and pantoprazole was suspended. A slow infusion of normotonic saline and magnesium sulfate was initiated to correct hyponatremia and hypomagnesemia.
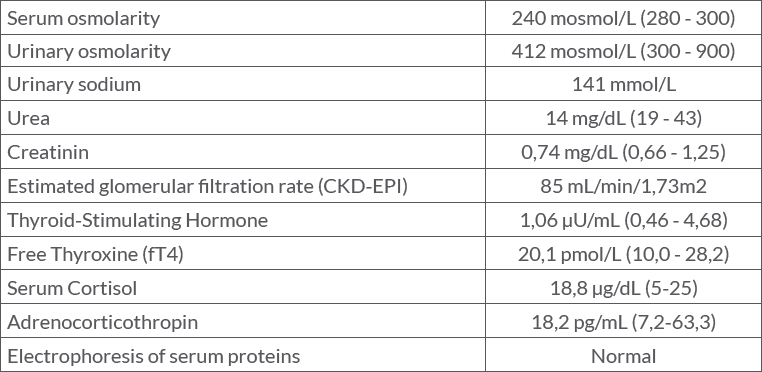
Table 1 summarizes the patient’s blood analysis, which revealed an effective serum osmolality inferior to 275mOsm/L (240 mOsm/L), which excluded non-hypotonic causes of hyponatremia. A urinary osmolality concentration above 100mOsm/L (412 mOsm/L) associated with a concentration of urinary sodium concentration of 141 mmol/L is consistent with inappropriate excretion of sodium by the kidney. SIADH was considered the appropriate diagnosis in this case, due to the euvolemic state and there was no prior use of diuretics, nor adrenal, thyroid, pituitary or renal insufficiency. In order to exclude cancer and diseases of the lung and central nervous system known to be associated with SIADH, a neck, thoracic, abdominal, pelvic and brain CT scan was performed and revealed no significant alterations. Considering the possibility of a drug-induced SIADH, after reviewing the patient’s medication, pantoprazole was considered o be the culprit. The patient was discharged with a serum sodium of 130 mmol/L and maintained the suspension of pantoprazole.
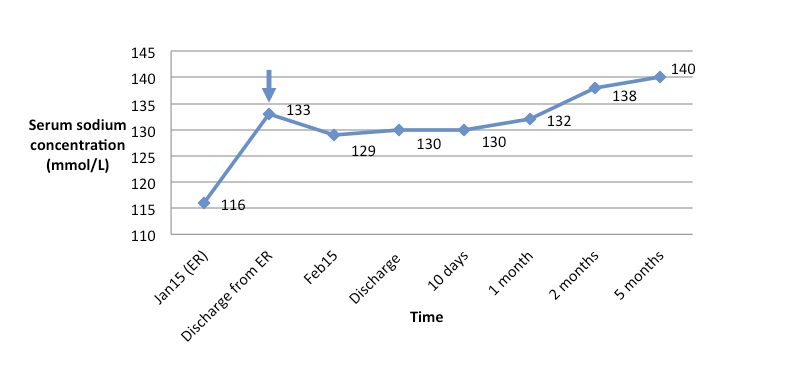
In the first revaluation, 10 days after discharge, he maintained a serum sodium of 130 mmol/L. In follow-up consultations, one, two and five months after discharge, the patient was asymptomatic and serum sodium was found to be in normal values, as shown in Fig. 1.
According to Naranjo Criteria5, there is a possible relation between hyponatremia and pantoprazole in this case report.
Figure 1: Evolution of sodium concentration. Arrow: pantoprazole suspension
DISCUSSION
Hyponatremia related to use of proton-pump inhibitor (PPI) therapy was usually described as a rare adverse drug reaction. More recently, in association with the widespread use of this medication in the last decade, it has been found more often than previously thought, despite the few reports in literature.
Real incidence of PPI-related hyponatremia in the elderly is unknown, but several studies concluded that the chronic use of PPIs increases the risk of hyponatremia and it is thought to be one of the most common causes2. Most patients with hyponatremia related to PPIs have mild symptoms, including nausea and confusion, while in the case reported by the authors the patient had severe manifestations such as vomiting and neurologic manifestations, with lentification and disorientation.
Most reported cases of hyponatremia due to PPIs are related with omeprazole3,4. In such cases, treatment with supplementation of sodium and/or water restriction revealed not being enough to improve hyponatremia until the treatment with omeprazole is discontinued3,4. Furthermore, there is one case reporting symptoms reappearance when the patient was re-challenged with the drug3. More recently, there were also reports of hyponatremia related to esomeprazole and pantoprazole4,5. In the case of the latter, a frail elderly adult achieved normal serum sodium levels three months after stopping treatment with pantoprazole5. In our case, serum sodium levels reached normal values two months after the suspension of pantoprazole.
The underlying pathophysiological mechanism of hyponatremia related to PPIs is not entirely clear and it is thought to be caused by SIADH. An excessive loss of urinary sodium seems more probable than water retention alone, but causality between PPI-induced hyponatremia and renal salt wasting has not been definitively proven3-5. This relation was found to be difficult to assess since this adverse drug reaction is generally encountered in elderly patients, who also have physiologic changes in water and electrolyte balance that occur as part of the normal aging process4. Some of the cases of hyponatremia related to Omeprazole met the criteria of SIADH, as well as the esomeprazole and pantoprazole-related cases. In these cases, the clinical use of Naranjo probability scale indicated a possible relation between hyponatremia and PPI3-5.
Although described in the past as a relatively innocuous drug in patients with no clinical indication and no benefits from PPI use, side effects may occur. It is paramount for physicians to re-evaluate the need for continuation of long-term therapy, considering the risk-benefit ratio as well as cost-effective prescribing practices.