ABSTRACT
Introduction: Gaucher disease (GD) is a rare inherited lysosomal storage disease characterized by multi-system impairment. One of its main features is the over-expressed chronic stimulation and activation of the immune system, which may play a crucial role in the development of some malignancies associated with GD.
Case Description: We describe a young woman diagnosed with GD type 1 in early adulthood who developed early-onset colorectal cancer shortly after GD diagnosis and the initiation of enzyme replacement therapy. She underwent radical surgical resection of the colon and adjuvant chemotherapy due to metastatic disease in the liver. She failed first-line therapy with capecitabine and is currently being treated with irinotecan plus the monoclonal antibody cetuximab.
Discussion: Although there is no evidence of an association between GD and colorectal cancer, this presentation in a young woman without a family history or risk factors may indicate a link. During anticancer treatment, only grade 3 anaemia was documented and no other haematological toxicities were observed. Enzyme replacement therapy at the recommended dose is regularly administered at scheduled intervals. The dosage may be increased in future if necessary to alleviate profound cytopenia.
Conclusion: Anticancer treatment in patients with GD can be challenging due to the accompanying cytopenia. Optimal treatment of these patients with cancer requires greater understanding of the pathophysiology of GD and its impact on haematopoiesis.
LEARNING POINTS
- There may be a correlation between the hyperinflammatory background of untreated Gaucher disease and the development of neoplasia.
- Gaucher disease has rarely been described in association with colorectal cancer.
- Gaucher disease can be further worsened by chemotherapeutic agents.
KEYWORDS
Gaucher disease, colorectal cancer, enzyme replacement therapy
INTRODUCTION
Gaucher disease (GD) was first described in 1882 and is a common lysosomal storage disease seen most frequently in Ashkenazi Jews. The condition is caused by a deficiency in the enzyme β-glucocerebrosidase, which plays an essential role in lipid catabolism by catalysing the hydrolysis of the β-glycosidic bonds in glucocerebroside [1]. The enzyme deficiency leads to accumulation of glucocerebroside in the cells of monocyte/macrophage lineage. These lipid-laden macrophages, known as ‘Gaucher-cells’, infiltrate various organs, especially the liver, spleen and bone marrow. The macrophage activation leads to an over-expressed systemic inflammatory response, which may play a critical role in the development of some malignancies, especially haematological malignancies. Compared with the general population, patients with GD type 1 are six times more likely to develop multiple myeloma (MM). However, a large analysis of the Gaucher Registry demonstrated that patients with GD were not at increased risk of other haematological malignancies or solid tumours [2].
We present the case of a woman in her late 30s with GD type 1, who was diagnosed with colorectal carcinoma very shortly after GD diagnosis and the initiation of enzyme replacement therapy (ERT).
CASE DESCRIPTION
A previously healthy 38-year-old woman was referred to our institution due to anaemia, thrombocytopenia and spleen enlargement. She complained of occasional bone pain in the pelvis, spine and ribs. She is the third and the youngest child in her family, born to a non-consanguineous marriage, and her family history is unremarkable for haematological or hereditary diseases.
On physical examination, the patient was pale with no signs of muco-cutaneous haemorrhage. She had splenomegaly with a palpable spleen notch 5 cm below the right costal margin, while the liver was not palpable. A spleen diameter of 19.5 cm was measured by abdominal ultrasonography. Initial laboratory tests revealed mild normocytic anaemia (103 g/l) and moderate thrombocytopenia (76×109l). Leucocytes were within normal ranges (WBC 6.6×109l). No significant changes in biochemical parameters were observed.
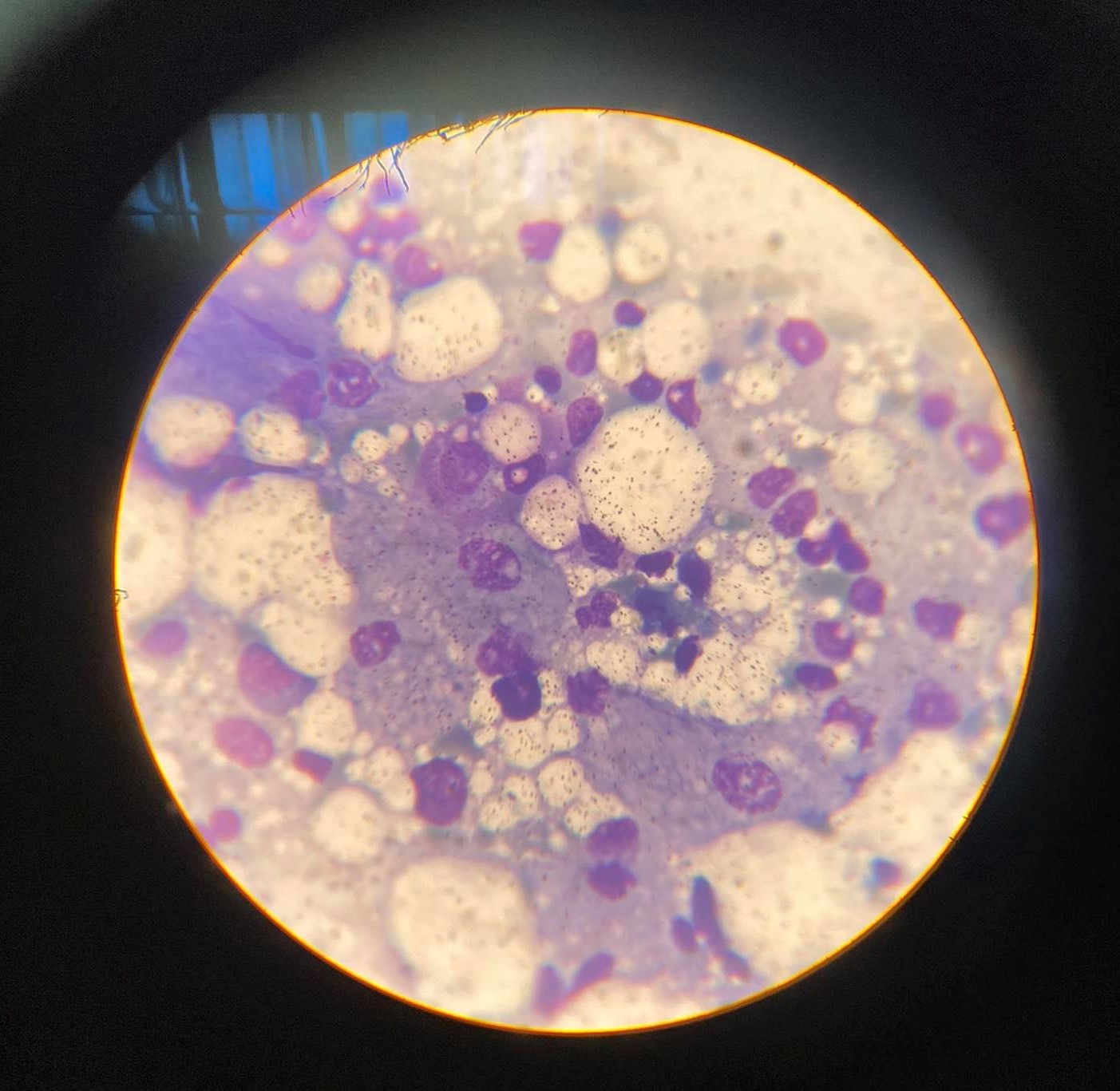
Due to suspicion of primary haematological disease, a bone marrow biopsy was performed, revealing infiltration of up to 30% Gaucher cells (Fig. 1). Molecular testing for GD was performed and a homozygous mutation in the GBA gene was detected: c.[226A>G] (as per cDNA nomenclature), traditionally known as N307S. The patient’s sister was subsequently diagnosed with GD and carrying the same genotype, while her brother was a GD carrier. An initial DEXA scan showed significant osteopenia. ERT with taliglucerase alfa was initiated at a dose of 60 units/kg once every 2 weeks. At 12 months, platelet counts reached a stable plateau of >100×109l, while mild anaemia was consistently observed.
Figure 1. May-Grünwald-Giemsa-stained bone marrow touch smears observed on light microscopy, showing bone marrow infiltration with up to 30% Gaucher cells. The presence of Gaucher cells is the pathological hallmark of Gaucher disease. Under light microscopy, these cells are seen as large cells with a diameter of 20–100 µm, with an eccentrically located nucleus with condensed chromatin. The cytoplasm is typically abundant, grey to sea-blue in colour, and foamy with numerous vacuoles, with a wrinkled tissue paper-like appearance.
At 14 months, the patient started experiencing left abdominal discomfort and constipation, necessitating further diagnostic procedures, and she was diagnosed with colorectal adenocarcinoma at the age of 40. She underwent radical surgical resection of the colon. Initial imaging demonstrated a solitary hepatic metastatic lesion and metastatectomy was planned but delayed due to the occurrence of a new lesion. The patient was referred to The University Clinic of Radiotherapy and Oncology and received three cycles of adjuvant chemotherapy with capecitabine. However, she failed capecitabine treatment and the CT scan performed at 4 months of treatment showed lesion progression in size. Second-line therapy was initiated: cetuximab, a monoclonal antibody inhibing the epidermal growth factor receptor, plus irinotecan was added from the third cycle of chemotherapy onwards. Cetuximab was administered at the dose of 500 mg/m2, irinotecan at a reduced dose of 120 mg/m2 , both every 2 weeks. A control CT scan at 6 months of treatment demonstrated a significant reduction in tumour masses. The same regimen is currently being followed.
The patient is monitored at our institution on a regular basis. ERT at the recommended dose is administered every 2 weeks. During a follow-up period of 9 months, the patient has received blood transfusions on two occasions. WBC counts have remained within the reference range. Platelets counts were between 90×109l and 120×109l. The last CT showed a reduction in spleen diameter to 16 cm.
DISCUSSION
In research published in 1993, GD was associated with an increased incidence of haematological malignancies [3]. A later and more extensive observational study of 505 GD patients did not find a significant excess risk for cancers compared with age-matched healthy individuals, except for MM [4]. This finding was further confirmed in a study from The International Gaucher Disease Registry, which included 2742 patients [2]. A multicentre study in Western Europe also observed an increased incidence of hepatocellular carcinoma [5]. Colon cancer has not been recognized in association with GD, and only sporadic cases have been published. This is in part due to the high global incidence of this cancer, so it is generally considered a coincidental finding. According to GLOBOCAN 2020 data, there were more than 1.9 million estimated cases of colorectal cancers worldwide in 2020. However, a red flag in our patient was the early onset of cancer in the absence of a family history and other risk factors; the GLOBOCAN 2020 data assess that the median age of diagnosis for colon cancer in women is 72.
Chemotherapy and biological therapy in patients with GD is challenging due to haematological toxicity and possible worsening of pre-existing cytopenia, which often requires chemotherapy dose reduction. Several trials have demonstrated that the addition of cetuximab to chemotherapy may increase the risk of grade 3 or higher haematological toxicity events (HTE). In our patient, grade 3 anaemia only was demonstrated and no other grade 3 or higher HTEs were noted. The recommended dose of ERT is regularly administered to our patient. In future, we may consider a dosage increase in ERT if necessary to alleviate more profound cytopenia.