ABSTRACT
Critically ill patients admitted into the intensive care units are susceptible to a wide array of complications that can be life-threatening, or lead to long-term complications. Some complications are inherent to the patient’s condition and others are related to therapeutics or care procedure. The prolonged prone positioning and mechanical ventilation devices are the first risk factors for orofacial complications. We report the case of a 47-year-old male patient, with a history of sleep apnoea syndrome, morbid obesity (body mass index of 43 kg/m2), and gastroesophageal reflux disease, presented to the emergency department with recent otorhinolaryngological symptoms of dysphonia and exertional dyspnoea lasting two days, and complicated with Quincke’s disease. First-line treatment consisted of a compilation of intravenous antihistamines and corticosteroids. The patient’s condition worsened. He developed an acute respiratory distress syndrome secondary to ventilator-acquired pneumonia with prone positioning ventilation, complicated by severe macroglossia. Soaked gauze dressings were placed around his tongue. Progressively, the size of his tongue reduced.
LEARNING POINTS
- Intensive care unit (ICU) patients are susceptible to a wide array of life-threatening complications that can be linked.
- Oral severe acquired Quincke’s disease is an isolated form of angioneurotic oedema that is induced by several factors including gastroesophageal reflux disease, sleep apnoea, inhalation exposure, or drug reactions. Macroglossia is rare life-threatening complication due to prolonged prone positioning of unknown pathogenesis. An experienced critical care staff with standardised protocol is needed to prevent such a complication.
- Because of possible consecutive severe orofacial complications, prolonged prone positioning for management of acute respiratory distress syndrome (ARDS) is not recommended in patients with inaugural oral angioedema.
KEYWORDS
Intensive care unit, Quincke’s disease, acute respiratory distress syndrome, macroglossia, prone positioning
INTRODUCTION
Patients admitted to the intensive care unit (ICU) are susceptible to a wide array of complications that can be life-threatening. Some complications are inherent to the patient’s condition and others are related to therapeutics or care procedure [1]. In acute respiratory distress syndrome (ARDS) patients, the change from the supine to the prone position markedly improves the arterial blood gases (ABGs) with a better overall ventilation/perfusion matching. The most frequent reported adverse events due to this manoeuvre are pressure sores and facial oedema [2]. We report the case of a patient with oral pressure urticaria followed by severe macroglossia due to prolonged prone positioning for management of ARDS.
CASE DESCRIPTION
A 47-year-old male patient native from Democratic Republic of Congo presented with a history of sleep apnoea syndrome, morbid obesity (body mass index 43 kg/m2), and gastroesophageal reflux disease. He denied any history of arterial hypertension and did not take any angiotensin-converting enzyme (ACE) inhibitors. He presented to the emergency department with recent otorhinolaryngological symptoms of dysphonia and exertional dyspnoea lasting two days. The physical examination showed a temperature of 38.5°C, oropharyngeal swelling with almost obstructive tonsils, major oedema of the uvula, and oedema of the lips. Blood pressure was 120/80 mmHg, heartbeat 100 bpm; pulmonary auscultation and abdominal palpation were normal. Laboratory findings in the emergency department showed negative nasal swab sampling for SARS-CoV-2 and negative anti-S SARS-CoV-2 serology, normal blood cell count, and elevated C-reactive protein of 85 mg/dL (normal range <5 mg/dL). First-line treatment consisted of nasal oxygenation, intravenous (IV) methylprednisolone (120 mg b.i.d), IV dexchlorpheniramine (5 mg t.i.d), and IV amoxicillin-clavulanate (1g /125 mg t.i.d).
The patient’s condition worsened rapidly by the development of ARDS, for which he was transferred to ICU, then intubated and mechanically ventilated. ABGs showed a respiratory acidosis with a pH of 7.24, PCO2 of 45 mm Hg, HCO3− of 27.5 mmol/L, PO2 of 61.60 mmHg, and oxygen saturation of 68.9%. At admission, a computed tomography (CT) scan showed a thickening of major adenoids, palatine tonsils, and uvula, markedly narrowing the nasopharyngeal canal. A second-line treatment of sub-cutaneous injections of icatibant was empirically administered (30 mg; two injections given 6 hours apart). On the 10th day of hospitalisation, the patient needed long-term airway support and received a tracheostomy. Thus, he developed an ARDS secondary to ventilator-acquired pneumonia due to cephalosporin-resistant strains of Klebsiella pneumoniae. The management consisted of 7-day course of IV piperacillin/tazobactam (4 g q.i.d), vasopressor support, and curarisation with prone positioning for a total period of 6 days. The patient was placed in prone positioning for 16 hours a day with mobilisation of the head and massage of pressure points every three hours to prevent skin laceration. During prone positioning, cushions were placed under the forehead, the torso, and the legs to avoid pressure points. Macroglossia was noted on day 6 (Fig. 1). A second neck CT showed homogenous tongue enlargement. Neither thrombosis nor neoplastic compressive processes were objectified (Fig. 2).
Figure 1. Macroglossia due to prolonged prone positioning for management of ARDS (on day 6 of hospitalisation in the ICU).
Figure 2. (A) Neck CT enhanced (sagittal facial view) showed an important enlargement of the tongue occupying the oral cavity and protrusion between the upper and lower lips, with no evidence of tumour or pathological enhancement. (B) Coronal maximum intensity projection (MIP) images showed cervical vessels permeability with no evidence of arteriovenous malformation.
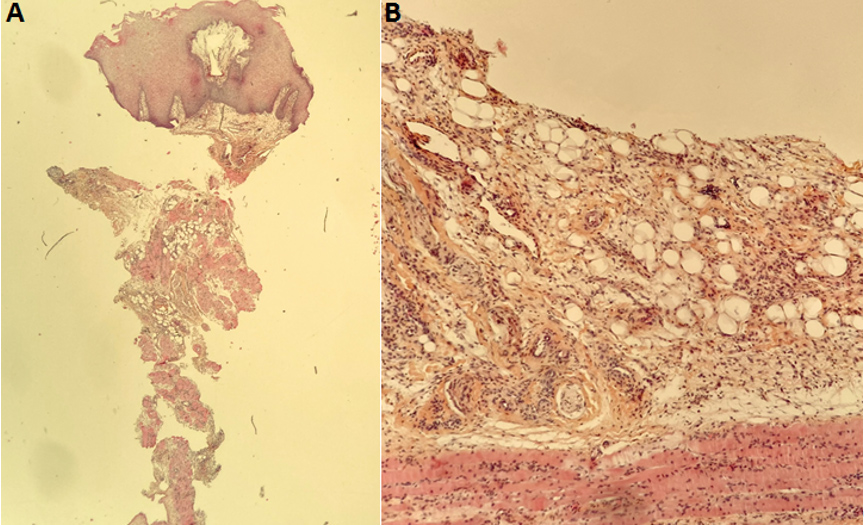
C1 inhibitor dosage was at 0.25 g/L (normal range 0.15–0.35 g/L). The patient was referred to the ear, nose and throat (ENT) specialist. The endoscopic assessment did not show any infection of neoplastic process and a biopsy was performed, which showed regular squamous epithelium without cytological or architectural abnormalities. Chorion-marked oedema dissociating the fibroadipose tissue with lymphatic capillaries hyperplasia was objectified. No vasculitic process, granuloma, amyloid deposits, lymphatic, or histiocytic infiltrate were identified. An immunohistochemistry study showed hyperexpression of CD34 compatible with hyperplasia of lymphatic vessels, scattered B-lymphocytes, and a majority of T lymphocytes on CD3 immunohistochemical staining without phenotypic abnormalities. Moreover, CD1a and PS 100 were negative (Fig. 3) and the cavum biopsy was normal. Severe macroglossia related to prolonged prone positioning for management of ARDS was diagnosed. Soaked gauze dressings were placed around the patient’s tongue and covered with tubular elastic dressing for graded, even compression, which was suspended by two strings to facilitate drainage through the normal venous and lymphatic channels. The tongue compression was applied for only 12 hours a day and did not cause any tongue injury.
Figure 3. (A) Light microscopy using haematoxylin-eosin saffron (HES) staining (×25) of tongue biopsy showed regular squamous epithelium with chorion-marked oedema without cytological or architectural abnormalities. (B) Light microscopy using HES staining (×100) confirmed chorion-marked oedema dissociating the fibroadipose tissue with lymphatic capillaries hyperplasia was objectified, with no vasculitic process, granuloma, amyloid deposits, lymphatic, nor histiocytic infiltrate.
By day 21, the size of the tongue was significantly reduced and at day 41, the patient was able to move his tongue and to intermittently retract it within the mouth. The patient was discharged on oral antihistamines; at 6 months’ follow-up, he remained symptom-free.
DISCUSSION
This clinical case illustrates that critically ill patients admitted to ICU are susceptible to a wide array of complications that can be life-threatening or lead to long-term complications. The oral mucocutaneous complications require multidisciplinary management and awareness of physician managing these conditions [3,4].
Our patient developed two successive acute oral complications. We first observed Quincke’s disease; this is a rare presentation of angioneurotic oedema affecting only the upper airway. Various etiological factors such as gastroesophageal reflux disease, sleep apnoea, inhalation exposure, drug reactions, and trauma have been implicated, thus provoking orofacial oedema [5]. Moreover, it can be a lethal complication of ACE inhibitors therapy and the emergency physician should focus on airway evaluation and management when treating patients with ACEi-induced angioedema [6].
In a context of therapeutic emergency, the patient received empirically icatibant injections with the hypothesis of bradykinin-mediated angioedema. The non-improvement of symptoms and normal C1-inhibitor dosage ruled out this hypothesis. Moreover, CT scan imaging ruled out other possible conditions such as local infection, tumour, or thrombosis. The management of Quincke’s disease is challenging. Antihistamines, the first-line and only approved treatment, are often not effective [7]. Other possible alternatives are parenteral and inhaled corticosteroids, beta-2 mimetics such as albuterol/salbutamol, and nebulised or topical epinephrine.
In our case, numerous treatments were administered but were unsuccessful. The patient’s condition worsened. He developed an ARDS and needed prone positioning ventilation in addition to standard care. Thus, he developed severe macroglossia. Histological examination showed chorion-marked oedema dissociating the fibroadipose tissue with lymphatic capillaries hyperplasia.
Macroglossia consists of painless enlargement of the tongue, which protrudes beyond the alveolar ridge or teeth. Its etiological spectrum is large and depends on whether it is an infiltrative condition, trauma, vascular, or lymphatic malformation. The etiological spectrum of acquired macroglossia is protean and includes hypothyroidism, protrusive neoplastic process, infiltrative conditions such as amyloidosis, acquired angioedema, and venous thrombosis [1]. More recently, macroglossia in COVID-19 patients not related to angioedema has been reported [8].
Severe macroglossia due to prolonged prone positioning has been reported after posterior fossa and craniofacial surgery. It can be a life-threatening condition due to upper airway obstruction if adequate precautions are not followed [9].
Prone positioning has been used as procedure for patients with acute lung injury or ARDS. This manoeuvre consistently improves systemic oxygenation in 70% to 80% of patients [10].
It is not a benign procedure and notable complications can arise resulting from localised pressure over the contact areas of the face, eyes, and periocular areas due to malpositioning. However, with standardised protocol and a trained and dedicated critical care staff, prone positioning can be performed safely [11]. Macroglossia is an extremely rare complication of this procedure. Little is known about the pathogenesis but mechanical obstruction of lymphatic, venous, and arterial flow, local ischaemia, and reperfusion injury could play a role [12,13].
In our case, pathological findings showed marked lymphatic capillaries hyperplasia, probably due to mechanical obstruction. The treatment consisted of tongue compression via soaked gauze dressings covered with tubular elastic dressing for graded with progressive positive improvement.
CONCLUSION
Quincke’s disease and macroglossia secondary to prolonged prone position are two rare orofacial complications in ICU patients. The management of these conditions is challenging and suffers from the lack of efficient treatment and recommendations. Nevertheless, we highlight the efficiency of tongue compression. Further, more extensive studies are needed to establish guidelines to this life-threatening complication.