ABSTRACT
Introduction: Primary vaginal malignant melanomas are rare tumours with a limited number of cases published in the literature. They primarily affect post-menopausal women with a median age of 57–68 years and have a dismal prognosis. The 5-year survival rate, regardless of treatment, is approximately 5–25%.
Case Description: We present the case of an 87-year-old female who presented with haematuria and urinary incontinence. She was diagnosed with AJCC stage IIIC vaginal melanoma. Considering her age and the extent of malignancy, surgery was not a viable option and immunotherapy with nivolumab and ipilimumab was initiated as treatment.
Discussion: The diagnosis of vaginal melanomas includes pathological analysis and immunohistochemistry (IHC) of the mass, imaging to determine extent, and genetic testing. Surgery is the preferred treatment in suitable cases. For metastatic or unresectable cases, immunotherapy or targeted therapy is the preferred first-line treatment. Due to the lack of an adequate number of cases to conduct randomized clinical trials, prognostic factors and treatment protocols for vaginal melanomas are not clearly defined. At present, the management of these tumours is largely based on retrospective studies and anecdotal evidence accompanied by significant knowledge gaps. Our case will be a valuable addition to the existing literature on vaginal melanomas that are managed non-surgically.
LEARNING POINTS
- Vaginal melanomas are extremely rare entities that require early diagnosis to ensure the best prognosis.
- Providers need to stress the importance of elderly gynaecological examination so crucial diagnoses are not missed.
- Further research is necessary to develop the most effective treatment plan for vaginal melanomas.
KEYWORDS
Vaginal melanoma, vaginal mass, haematuria, gynaecology, urology, oncology
CASE DESCRIPTION
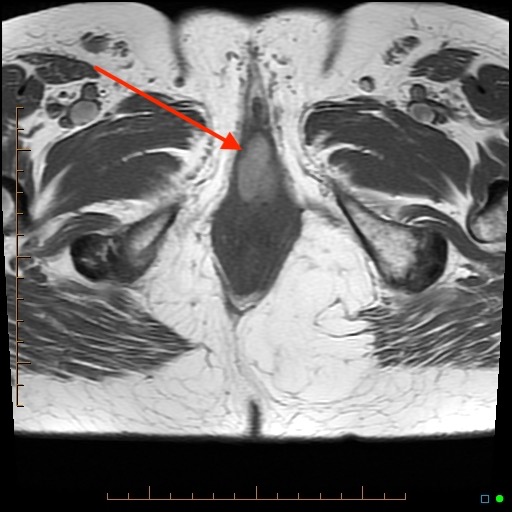
An 84-year-old woman presented to the Urology clinic with worsening haematuria and urinary incontinence for 2 months. Physical examination including the external genitalia was grossly normal. An attempt to perform flexible cystoscopy revealed a large, friable, dark-blue mass arising from the vagina covering the urethra. A detailed gynaecological examination showed a large, dark-blue mass protruding around 3 cm out of the vagina (Fig. 1) and speculum examination visualized it arising from the anterior vaginal wall. The upper anterior vagina had blue streaks concerning for lymphatic involvement. The rest of the vaginal examination was normal. A uterine exam was not performed as the patient had undergone a hysterectomy. Apart from mild anaemia, her laboratory results were unremarkable. Contrast-enhanced magnetic resonance imaging (MRI) of the pelvis showed a 3.2×1.7×2.6 cm lesion in the perineum (Fig. 2) along with a 2.3×1.4 cm right inguinal lymph node.
Figure 1. Clinical image taken during examination under anaesthesia.
Figure 2. Pelvic MRI (T1 axial view) showing a large mass in the vagina. The lesion demonstrates an elevated signal on T1, which is common for melanomas.
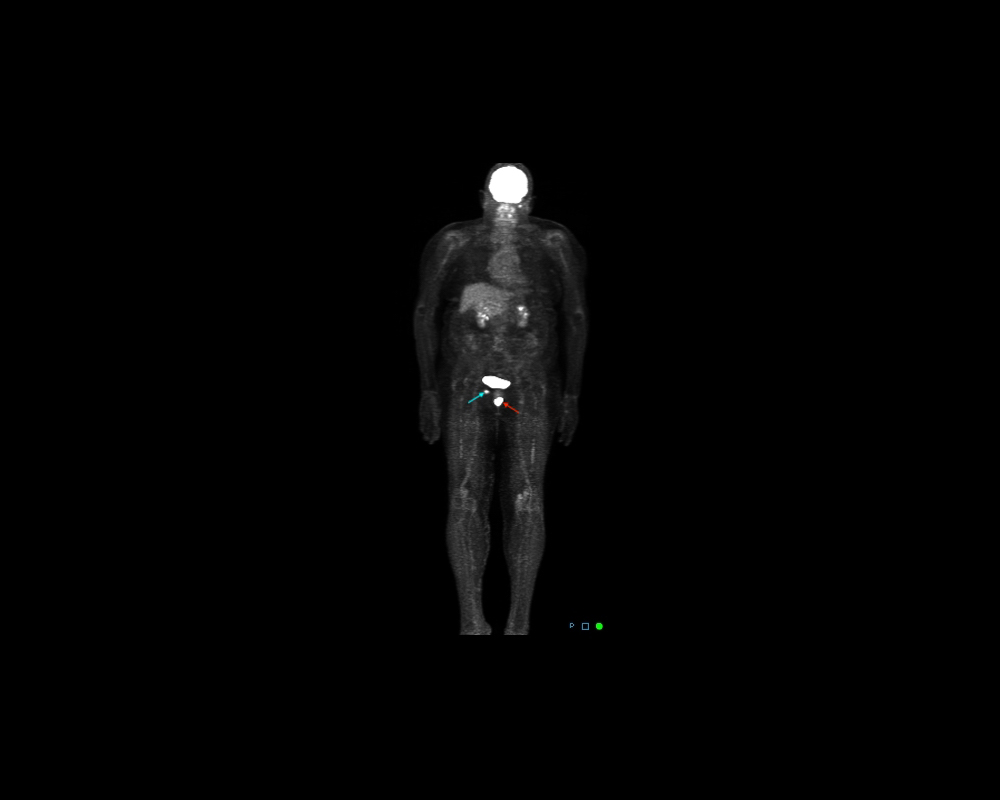
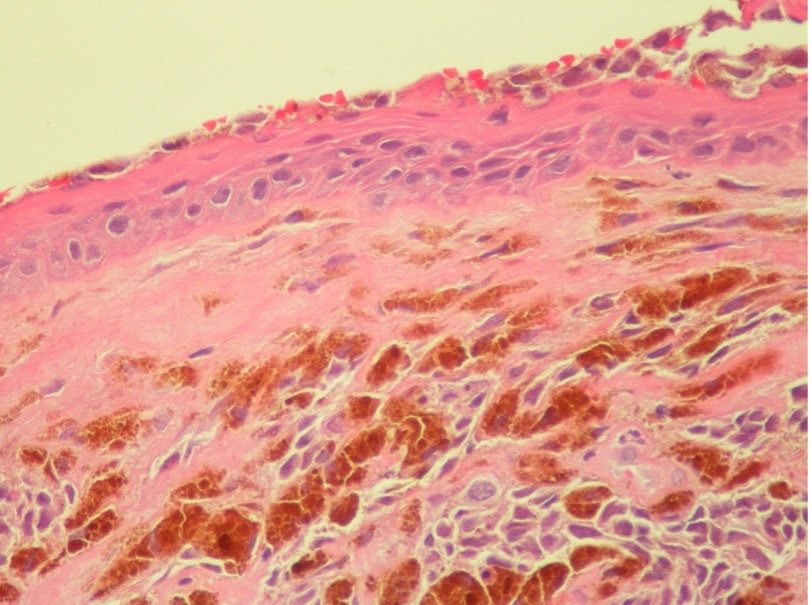
A whole-body positron emission tomography (PET) result corroborated the MRI findings (Fig. 3). It demonstrated a focal lesion of markedly elevated metabolic activity in the inferior vaginal region, slightly right of the midline, along with elevated metabolic activity in a right inguinal lymph node. The patient underwent pelvic examination under anaesthesia coupled with an incisional biopsy of the vaginal mass and cystourethroscopy. Tumour seeding was noted in the distal posterior urethra, with the rest of the exam being normal. Subsequently, an ultrasound-guided biopsy of the right inguinal lymph node was performed. The vaginal mass biopsy (Fig. 4) was reported as invasive melanoma with a Breslow’s thickness of 4.5 mm, no ulceration, invasion present at the margin, a mitotic rate of 3/hpf (high power field), no microsatellitosis, and no lymphovascular invasion, neurotropism or tumour regression. Immunohistochemistry (IHC) was positive for BAP1 and Melan-A. Concurrently, the inguinal node biopsy was reported as metastatic melanoma. Genetic testing on the biopsy showed no mutations in the BRAF, NTRK, NRAS or c-KIT genes. Thus, the patient was diagnosed with invasive vaginal malignant melanoma classified as FIGO stage III and pathological stage IIIC - T4a N1a Mo as per the American Joint Committee on Cancer (AJCC) prognostic stage groups. After a multidisciplinary discussion at the institutional tumour board meeting, the patient was deemed to be a poor surgical candidate considering her age and the extent of malignancy. She was started on immunotherapy with nivolumab and ipilimumab. She completed the first cycle with good tolerance and continues to follow up with us.
Figure 3. Maximum imaging projection (MIP) of a PET/CT scan showing the vaginal mass (red arrow) and right inguinal lymph node (blue arrow). The unlabelled, high activity area in the pelvis represents the bladder, which is a normal finding.
Figure 4. Histopathology of the vaginal mass biopsy.
DISCUSSION
Melanoma is a highly aggressive tumour of melanocytes originating most commonly in the skin and to a much lesser extent in other areas like the eyes and mucosal membranes. Mucosal melanomas (MM) account for 1% of all melanomas and 18% of these arise in the vulvovaginal regions[1]. The incidence of genital melanomas is 1.74 per million women and the peak incidence of vaginal melanoma occurs between 57 and 68 years of age. Vaginal melanomas most commonly occur in the anterior wall of the lower third of the vagina, as in our case. Given the rarity of vaginal melanomas, there are no clear identifiable causative factors. Chronic inflammatory conditions, irritant chemicals, and viral infections are thought to be contributory[2,3]. There is no evidence that HPV infection predisposes to vaginal melanomas. In general, the female gender appears to be a risk factor for MM, as they are twice as common in women compared to men. In contrast, cutaneous melanoma (CM) distribution is similar between both genders[4]. Additionally, certain genetic alterations are found to be associated with MM: activating mutations in SF3B1 and KIT, loss of CDKN2A, PTEN or SPRED1, and amplification of CDK4, TERT, KIT, MDM2 or CCND1. Unlike CM, BRAF and NRAS mutations are less frequent in MM[2]. Gene sequencing of MM helps identify driver mutations and provides therapeutic opportunities for targeted therapy. The most common presenting complaint of vaginal melanomas is genital bleeding, while others include a palpable mass, itching, dyspareunia, yellow genital secretions, and local pain[4]. The diagnosis of vaginal melanomas includes pathological analysis and IHC of the biopsy sample, imaging to determine extent, and genetic testing. Histologically, vaginal melanomas are divided into three broad types: epithelioid (55% of cases), spindled (17%) and mixed type (28%)[5]. IHC can be helpful in difficult cases to confirm that the neoplasm is of melanocytic origin. Widely used markers include protein S-100, melanoma antigen recognized by T-cells-1 (MART-1) or Melan-A, melanoma-specific antigen (HMB-45), microphthalmia transcription factor (MITF), and vimentin[4]. Due to the lack of an adequate number of cases to conduct randomized clinical trials, prognostic factors and treatment protocols are not clearly defined for vaginal melanoma. At present, there is no standardized staging system that has been shown to be a useful predictor of prognosis. The 8th Edition of the AJCC staging manual emphasizes that there is no AJCC staging system for vaginal MM. Nevertheless, FIGO 2009 vaginal cancer staging may be used for vaginal melanoma as the vaginal section of the 2018 FIGO cancer report does not mention that MM should be excluded. The available evidence from different studies indicates AJCC stage, tumour size, and lymph node status as the major prognostic factors. AJCC stage ≥III, tumour size ≥3 cm, and lymph node involvement were associated with worse outcomes[3]. The 5-year overall survival rate of MM, in general, is 10–20%, compared with 93% for CM[2]. Moreover, the 5-year survival rates for vaginal melanoma (5–25%) are much lower than those for vulvar melanoma (24–77%)[6,7].
Owing to the lack of dedicated treatment guidelines, CM guidelines are often extrapolated to treat vaginal melanoma. Surgery is the preferred treatment modality in suitable cases as it is associated with increased overall survival. However, the radicality of surgery had no significant impact on outcomes. Distant metastasis was observed to occur irrespective of the extent of surgical resection[3]. Therefore, quality of life and patient preferences are vital in deciding the extent of surgery. Due to the low rate of regional lymph node metastasis, routine groin or pelvic lymphadenectomy is not recommended for patients without evidence of clinical or radiological involvement. Radiotherapy may be used as a neoadjuvant treatment to reduce tumour size to make surgical resection possible. For patients with positive or unclear surgical margins, tumour size ≥3cm, or regional lymph node involvement, radiotherapy can be considered as adjuvant therapy[3]. The preferable first-line therapy for metastatic or unresectable vaginal melanoma is immune checkpoint inhibitors or targeted therapy in the presence of driver mutations. Combination therapy with nivolumab and ipilimumab or anti-PD1 monotherapy with pembrolizumab or nivolumab are the recommended initial regimens[8–12]. Tyrosine-kinase inhibitors like imatinib and nilotinib are shown to be useful in cases with genetic C-KIT alterations and larotrectinib for NTRK gene fusion-positive patients[13–15]. Evidence shows that cytotoxic therapy has a limited impact on overall survival and is not a preferred first-line therapy[8,11,12]. Immunotherapeutic agents and genetically targeted drugs have replaced cytotoxic agents and interferon-α as adjunctive systemic therapy due to better tolerance and efficacy[16,17].
Vaginal melanomas are clinically rare malignancies that have a poorer prognosis than other vaginal cancers and CM[3]. At present, the management of these tumours is largely based on retrospective studies and anecdotal evidence accompanied by significant knowledge gaps. Our patient with a tumour size >3 cm and AJCC stage IIIC was started on nivolumab and ipilimumab in combination with a plan to administer four cycles followed by a restaging scan. This case will be a valuable addition to the existing literature on vaginal melanomas that are managed non-surgically.