ABSTRACT
Background: Massive haemoptysis is a rare symptom ofcoronavirus disease 2019 (COVID-19). Management can be very challenging due to the lack of clear recommendations.
Case description: We report a case of massive recurrent haemoptysis in a young patient who tested positive for COVID-19 with successful management using endovascular embolization.
Discussion: Life-threatening massive haemoptysis has rarely been reported as the only manifestation of COVID-19. Embolisation was the therapeutic option chosen to manage this emergency.
LEARNING POINTS
- Haemoptysis is a rare atypical presentation that can reveal COVID-19, highlighting the complexity of its pathogenesis.
- Atypical manifestations should raise suspicion for COVID-19.
- In this patient with COVID-19, life-threatening massive haemoptysis was successfully treated with endovascular embolisation.
KEYWORDS
COVID-19, haemoptysis, embolisation
INTRODUCTION
As the COVID-19 pandemic continues, physicians are still facing challenges to ensure adequate care for patients affected by this disease. The clinical spectrum ranges from asymptomatic to severe forms including acute respiratory distress syndrome. Patients commonly present with symptoms like fever, myalgia, fatigue, cough and dyspnoea. Other symptoms such as haemoptysis have also been occasionally reported[1]. In rare cases, patients have presented with massive haemoptysis requiring urgent endovascular management. However, very few studies have highlighted the use of arterial embolization in haemoptysis due to SARS-CoV-2 infection because of a lack of clear recommendations. We were confronted with such a situation, where massive recurrent haemoptysis was the unique symptom in a young patient who tested positive for the virus, with successful management using endovascular embolization.
CASE DESCRIPTION
A 23-year-old man presented to the emergency department in January 2021 with moderate haemoptysis of acute onset. He was a current smoker with no significant medical history. He had no fever, dyspnoea or cough. Physical examination and a chest radiograph were normal.
Baseline laboratory analysis was unremarkable, excluding haemostatic disorders.
We observed a normal prothrombin timeand fibrinogen levels, and no thrombocytopenia.
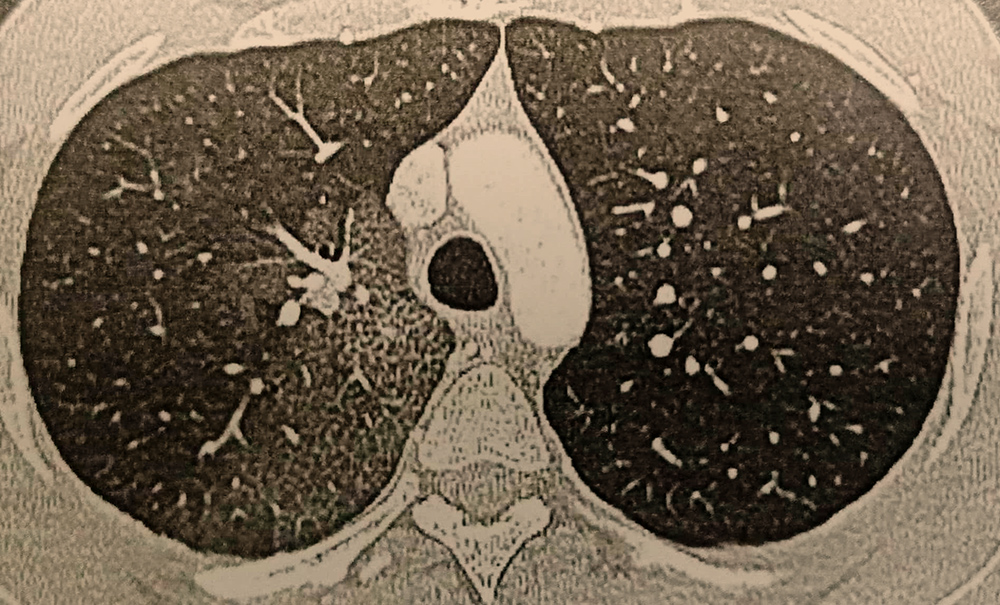
C-reactive protein and D-dimer concentrations were not elevated. Renal function and liver enzymes were normal. Anti-neutrophil cytoplasmic antibodies and antinuclear antibodies were negative. Given the COVID-19 pandemic, we obtained a nasopharyngeal swab sample, which was positive for SARS-CoV-2 by real-time polymerase chain reaction (RT-PCR). Chest computed tomography (CT) ruled out pulmonary embolism but suggested alveolar haemorrhage in the upper right lobe. No arterial blush or aneurysms were visualized (Fig.1).
Figure 1. Computed tomography scan of the thorax showing alveolar haemorrhage in the posterior segment of the upper right lobe
The patient was admitted and underwent flexible bronchoscopy to better explore possible haemoptysis. Staff wore personal protective equipment including an FFP2 mask, gown, goggles, shoe protection, and a face shield. Bronchoscopy showed active diffuse bleeding in the upper right lobe and numerous clots in the lower right lobe. Local iced saline and adrenaline solution were administered to control the bleeding. Broncho-alveolarlavage showed no bacterial or fungal infection.Because of the patient’s stable respiratory and haemodynamic status, conservative treatment was initiated using adrenaline aerosol and vasopressin. However, on day 3, the patient experienced massive life-threatening haemoptysis of up to 500 ml. The haemoglobin level fell to 8 g/dl, which required transfusion with 2 units of packed red blood cells.
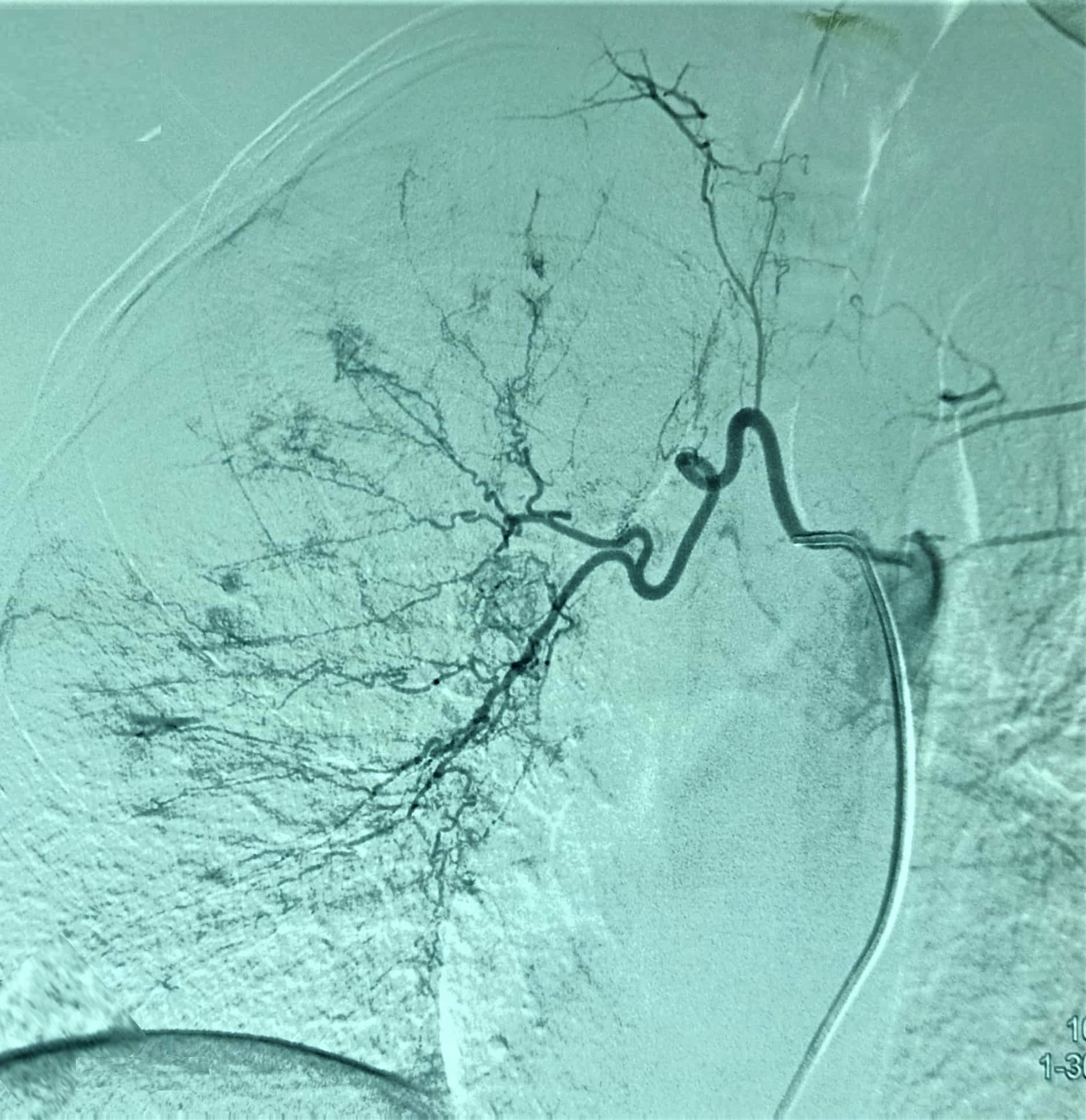
Faced with recurrent massive bleeding, bronchial angiography was immediately performed. The intercostal arteries were accessed via the right femoral artery and catheterized using a 6 French sheath. Catheterization of the right bronchial artery revealed a tortuous artery with diffuse dysplasia and multipledisseminated small focal areas of hypervascularization throughout the right lung (Fig.2).
Complete right embolization was performed using calibrated particles (Embozene® 500 μm/700 μm; Varian Medical Systems) with total devascularization of the right bronchial artery. An optimal post-procedure result was obtained (Fig. 3).
No further episodes of bleeding occurred after the procedure. However, our patient then presented acute abdominal pain. He underwent an abdominal angio-CT scan, showing multiple renal and splenic infarctions secondary to previous embolization. Oral and systemic hyperhydration was administered with full recovery without sequelae. Our patient was discharged with no recurrence of symptoms during the 6 months of follow-up.
Figure 2. Selective catheterization demonstrates a tortuous artery with diffuse dysplasia and multiple disseminated small focal areas of hypervascularization throughout the right lung
Figure 3. Total devascularization of the right bronchial artery after embolization
DISCUSSION
The emergence of SARS-CoV-2 resulted in the COVID-19 pandemic. The disease remains unpredictable and is characterized by a wide clinical spectrum. The most commonly reported symptoms and signs at onset are cough, fever, fatigue, ageusia and dyspnoea [2,3]. Haemoptysis has rarely been reported as a unique symptom of COVID-19 and is usually associated with COVID-19 pneumonia as a complication of embolism or coagulation therapy. The prevalence of haemoptysis was less than 1% in a meta-analysis that included 19 studies and a total of 2874 patients. Most of the reported cases of haemoptysis occurred early in the course of the disease with a prevalence of 2–3%. This symptom often results from thromboembolic disease or anticoagulation therapy [5].
The first patients with COVID-19 whose initial symptom was haemoptysis were described by Shi et al.[6] and Argun Barış et al.[5] . However, in our case, haemoptysis was the unique symptom during 21 days of hospitalization without any of the typical CT findings.The COVID-19 PCR testwas performed to exclude the diagnosis because the patient was hospitalized in a non-COVID-19 ward.
In light of the severity of haemoptysis in this case, we emphasize that haemoptysis could be a unique fatal manifestation of SARS-CoV-2 infection. The first case of COVID-19 associated with life-threatening haemoptysis was reported by Peys et al.[1], where alveolar bleeding was mentioned as a possible complication of COVID-19. Only a few cases of COVID-19 have been associated with massive haemoptysis in the literature. Argun et al.[5] described three patients with COVID-19 who were admitted with massive haemoptysis. Smoking and bronchiectasis may have contributed to the development of haemoptysis in these cases. A pulmonary artery pseudoaneurysm was also reported as another aetiology by Jajodia and colleagues [7].
A case of massive haemoptysis occurring as a delayed effectmonths after mild symptomatic COVID-19 disease was recently published [8].
The atypical manifestations indicate the complexity of the pathogenesis of pneumonia caused by SARS-CoV-2 infection. Haemoptysis is related to several mechanisms in COVID-19 disease. Indeed, post-mortem examination of 21 COVID-19 patients revealed diffuse alveolar damage with severe capillary congestion, pulmonary embolism, alveolar haemorrhage, and vasculitis in the lungs[9].
Haemoptysis can also be the initial symptom of venous thromboembolismcaused by the proinflammatory and hypercoagulable state triggered by SARS-CoV-2[10]. Casey et al.[11] reported a case of acute segmental pulmonary emboli associated with COVID-19 infection.However, in our patient,hypercoagulabilitywas ruled out by normal LDH, D-dimer and ferritin values, and non-venous thromboembolism was observed on CT scanning.
In conclusion, haemoptysis is a possible clinical presentation in COVID-19 although it is not common. Clinicians should be careful when patients present with respiratory symptoms of unknown aetiology.