ABSTRACT
Introduction: Delayed diagnosis of intravascular large B-cell lymphoma (IVLBCL) is associated with a poor prognosis, making early diagnosis and treatment essential. However, early diagnosis remains challenging.
Case description: Here we present the case of a 75-year-old man with fever of unknown origin, in whom random skin biopsy (RSB) allowed early diagnosis of IVLBCL.
Discussion: The usefulness of RSB, which involves incisional skin biopsies of three or more sites that contain subcutaneous fatty tissue, such as the thighs, abdomen and upper arms, has been debated. In cases of suspected IVLBCL, RSB is less invasive than a biopsy of the internal organs.
Conclusion: We suggest that combining RSB with bone marrow examination may facilitate the diagnosis of IVLBCL.
LEARNING POINTS
- Delayed diagnosis of intravascular large B-cell lymphoma (IVLBCL) is associated with a poor prognosis, but early diagnosis is difficult due to its diverse, non-specific presentation.
- This case report illustrates the value of random skin biopsy in the early diagnosis of IVLBCL in a man with fever of unknown origin and haematological abnormalities without lymphadenopathy, splenomegaly or bone marrow abnormalities.
- The diagnostic accuracy of random skin biopsy depends on several factors, including the location and number of sites biopsied, and the depth and width of the biopsy.
KEYWORDS
Intravascular large B-cell lymphoma, random skin biopsy, early diagnosis
BACKGROUND
Intravascular large B-cell lymphoma (IVLBCL) is a type of extranodal B-cell lymphoma in which tumour cells selectively grow in the small blood vessels of systemic organs. According to a European report, it is a rare disease with a prevalence of only 1 in 1 million, with no sex differences, and a median age at diagnosis of 70 years [1]. IVLBCL is difficult to diagnose because lymphadenopathy, a common feature of malignant lymphoma, is absent and because it presents with non-specific symptoms, such as fever, general malaise and respiratory symptoms. A delay in diagnosis leads to clinical deterioration and poor prognosis. In 2008, the disease was included in the fourth edition of the World Health Organization classification as an independent disease entity; however, it remains under-recognised due to the non-specific nature of its symptoms. When IVLBCL is suspected based on the symptoms and clinical examination, histopathology of tumour cells is useful, and a combination of bone marrow examination and random skin biopsy (RSB) is recommended. A retrospective study conducted in Japan revealed that 81% and 15% of cases of IVLBCL were diagnosed by bone marrow biopsy and skin biopsy, respectively, and that RSB was not widely used in diagnosis [1]. The sensitivity and specificity of RSB in the diagnosis of IVLBCL can be relatively high [2]; therefore, clinicians should consider RSB for early detection of IVLBCL.
CASE DESCRIPTION
A 73-year-old man presented to his local physician with a 1-month history of fever and a sore throat. Initially, he was diagnosed with a common cold and was prescribed antibiotics but later developed a recurrent fever of 38°C. After 1 week, he revisited his doctor and was treated with antipyretic analgesics; however, his high fever persisted. He subsequently developed pain in the peripheral joints and malaise, and was referred to our emergency department for a diagnostic investigation. A general fever work-up (general blood test, urine test, blood culture, chest radiography, and computed tomography scan of the chest and abdomen) in the emergency department did not reveal any obvious causes. The patient was referred to the general medical department for further evaluation. His medical and medications history was unremarkable.
Investigations
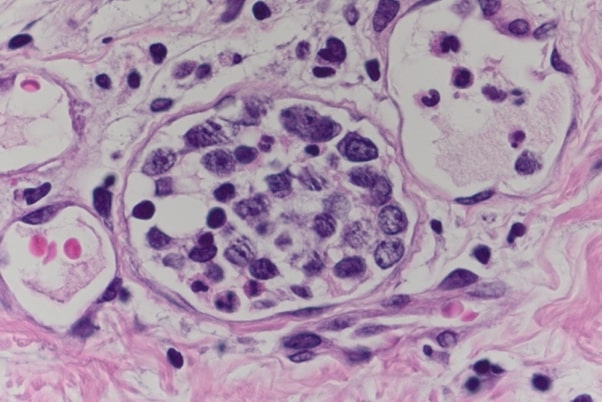
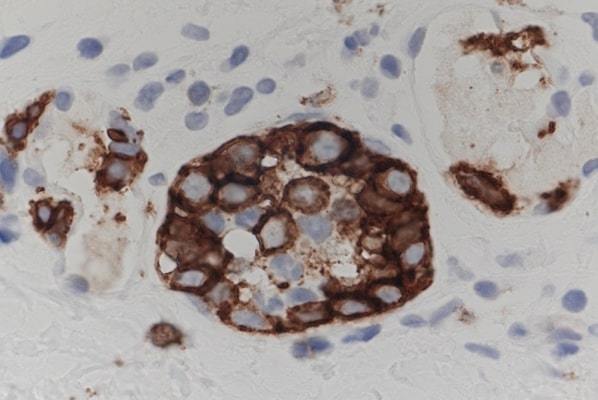
The patient’s vital signs were as follows: body temperature, 38.2°C; blood pressure, 143/68 mmHg; pulse, 90 beats/min; respiratory rate, 24 breaths/min. Physical examination revealed no abnormalities in the heart or respiratory sounds, and no skin abnormalities, such as erythema or purpura. Abdominal examination revealed hepatosplenomegaly, and no abnormalities were detected on neurological examination. A full blood count revealed leucocytosis (17,280/µl, normal: 3,300–8,600/µl) with neutrophil predominance (81.0%, normal: 45.5–69.8%); blood biochemistry revealed elevated levels of aspartate transaminase (AST) (185 IU/l, normal: 13–30 IU/l), alanine transaminase (ALT) (162 IU/l, normal: 10–42 IU/l), lactate dehydrogenase (LDH) (520 U/l, normal: 124–222 U/l), ferritin (1211.48 ng/ml, normal: 50–200 ng/ml) and soluble interleukin-2 receptor (sIL-2R) (3267 U/ml, normal: 122–496 U/ml). Contrast-enhanced computed tomography of the chest and abdomen revealed mild hepatosplenomegaly, but no pathological enlargement of the cervical, inguinal or axillary lymph nodes, and no abnormalities in the lung fields. A bone marrow biopsy and RSB were performed on the third day of hospitalization. Three skin biopsies were collected from normal-appearing skin of the left upper arm, abdomen and thigh, all of which showed tumour cells in the blood vessels of the subcutaneous adipose tissue (CD20-positive, CD3-negative, large atypical B lymphocytes) (Figs. 1 and 2). Based on the clinical presentation, blood test results, and the RSB histopathology, the patient was diagnosed with stage 4 IVLBCL. Brain magnetic resonance imaging was performed to search for central nervous system invasion, but no central nervous system lesions were detected.
Figure 1. Histopathology of a random biopsy specimen showing large atypical B lymphocytes in the lumen of the small blood vessels (haematoxylin and eosin stain, ×200)
Figure 2. Histopathology of a random biopsy specimen showing positive CD20 staining of the atypical B lymphocytes in the lumen of the small blood vessels (CD20 stain, ×200)
Differential diagnosis
Sore throat, hepatosplenomegaly, and elevated levels of AST, ALT, LDH, ferritin and sIL-2R, led us to consider viral infections such as Epstein-Barr virus, sepsis, miliary tuberculosis, haematological diseases such as intravascular lymphoma, and collagen diseases such as adult Still’s disease, systemic lupus erythematosus and polyarteritis nodosa as differential diagnoses.
Treatment
R-CHOP (rituximab 375 mg/m2, cyclophosphamide 750 mg/m2, doxorubicin 50 mg/m2, vincristine 1.4 mg/m2, prednisolone 40 mg/m2) therapy combined with high-dose methotrexate plus intrathecal chemotherapy was initiated on the sixth day of hospitalization. The patient received six courses of R-CHOP chemotherapy.
Outcome and follow-up
By the end of the third course, the patient’s fever, malaise and laboratory abnormalities, such as LDH and sIL-2R elevation, had improved. We performed bone marrow biopsy and RSB to evaluate the presence or absence of residual tumour cells. No invasion of tumour cells into the bone marrow was observed. RSB, from three areas near the initial biopsy sites, did not reveal tumour cells in any of the sites, and the patient was considered to be in remission. A complete response was achieved, and the patient has remained relapse-free a year after treatment.
DISCUSSION
IVLBCL is a rare type of lymphoma involving selective tumour growth in small blood vessels [1, 2]. Most of the previously reported cases have been B-cell (88%), T-cell (6%) and NK-cell (2%) lymphomas [3]. There are regional differences in the organs involved, and 60%, 8%, 11% and 7% of cases involve the central nervous system, skin, bone marrow and spleen, and lung, respectively [3, 4]. Several types of haemophagocytic syndrome with hepatosplenomegaly have been observed in Japan and other Asian countries. IVLBCL with haemophagocytic syndrome and hepatosplenomegaly, as described in this case, is termed the Asian variant. IVLBCL must be considered in the differential diagnosis when such findings are observed [5].
When IVLBCL is suspected, it is helpful to confirm the presence of tumour cells by histopathology, even if the localisation of tumour cells is not precise; furthermore, it is recommended to combine bone marrow examination and RSB. However, it is often difficult to determine the threshold for RSB in patients with fever of unknown origin without skin manifestations.
In Japan, retrospective studies on the diagnostic sites of IVLBCL have reported that 81% and 15% of cases are diagnosed based on bone marrow and skin findings, respectively [1]. However, Sitthinamsuwan et al. [6] reported that an RSB is particularly useful in diagnosing intravascular lymphoma in patients with one or more of the four following findings with fever of unknown origin: (a) haematological abnormalities, (b) elevated serum LDH levels, (c) hypoxaemia, and (d) abnormal neurological symptoms and haematological abnormalities, without lymphadenopathy or hepatosplenomegaly on physical examination or imaging, and no abnormalities on bone marrow examination. In this case, three of these findings were present, which led us to perform RSB.
An RSB is recommended in cases of fever of unknown origin without skin lesions when the above four criteria are present and intravascular lymphoma is suspected. Although skin biopsies have not been actively performed in Japan in the past because of the low incidence of skin lesions in Asians, their diagnostic value has been reconsidered in recent years because of the high incidence of tumour cells detected in apparently healthy skin [7]. With RSB, specimens are usually collected from three or more sites [8] and an incisional biopsy (with a depth of more than 5 mm from the skin surface) that includes fatty tissue is recommended instead of a punch biopsy. This is based on the report by Enzan et al. [9] that in 38 skin biopsies from patients with IVLBCL, the median minimum depth from the skin surface to the tumour cells was 3.64 mm, with 47% having a depth of 4 mm or greater and 37% having a depth of 5 mm or greater. However, when there is thrombocytopenia or coagulation abnormalities and biopsy complications are feared, a 4 mm punch biopsy may be used as an alternative [10]. In summary, this case illustrates the value of RSB in the early diagnosis of IVLBCL.