ABSTRACT
We describe four cases of COVID-19 infection during the Omicron wave, in patients treated with anti-CD20 monoclonal antibodies. All cases follow a similar biphasic clinical course consisting of respiratory deterioration, which occurred a few weeks after convalescence from initial mild to asymptomatic infection. Possible explanations are discussed.
LEARNING POINTS
- Four cases of COVID-19 infection in anti-CD20 treated patients are described.
- These cases display a unique biphasic course that was previously undescribed: respiratory deterioration weeks after convalescence.
- Awareness of such a course and rapid utilisation of bronchoalveolar lavage will lead to quicker diagnosis and more timely, appropriate treatment.
KEYWORDS
COVID-19, anti-CD20, rituximab, obinutuzumab, Omicron
INTRODUCTION
Anti-CD20 monoclonal antibodies are routinely used for treatment of haematological malignancies and autoimmune syndromes. Targeting CD20 depletes B cells, causing susceptibility to sinopulmonary infections and certain viruses. Since the emergence of COVID-19, data has been accumulated regarding an association of anti-CD20 treatment and COVID-19 infection course and severity. While initial studies suggested a protective effect for anti-CD20 treatment in COVID-19 infection [1], it is now well established that COVID-19 patients treated with anti-CD20 shed the virus for longer periods and develop severe disease in higher proportions [2]. Case reports written before the emergence of B1.1.529 (Omicron) described an atypical disease course with persistent symptoms for weeks and relapse shortly after resolution of initial symptoms [3,4]. Here we explore four cases of COVID-19 related lung disease in anti-CD20 treated patients, presenting during the Omicron wave in Israel.
These cases display a similar pattern of biphasic course: convalescence from mild infection, a symptom-free period during which they were defined as recovered, followed by the onset of respiratory symptoms with a progressive clinical course, development of respiratory failure, and a need for invasive or non-invasive positive pressure ventilation.
CASE SERIES
Patient 1
AAn unvaccinated 69-year-old woman with follicular lymphoma, treated with obinutuzumab as maintenance therapy. She was diagnosed with COVID-19 four weeks prior to admission by PCR. Treated with nirmatrelvir and ritonavir, she experienced asymptomatic disease and was considered convalescent with a negative PCR after one week. A week prior to admission she developed fever, throat soreness, and a cough. A chest x-ray was unremarkable, and antibiotics were initiated in primary care without improvement. On the morning of admission, she experienced micturition syncope. PCR for COVID-19 on admission was negative, and a chest x-ray revealed diffuse interstitial infiltrates. She continued to worsen despite treatment with ceftriaxone and ofloxacin, eventually requiring supplemental oxygen. Chest CT revealed ground-glass opacities (GGO) with a crazy paving pattern. Bronchoalveolar lavage (BAL) was positive for COVID-19 PCR. Treatment with dexamethasone and remdesivir was initiated but she continued to deteriorate, requiring intubation and transfer to the intensive care unit where she died a month after her admission.
Patient 2
A 42-year-old woman with multiple sclerosis, treated with rituximab and prednisone, vaccinated three times with BNT162b2. She was diagnosed with COVID-19 five weeks prior to admission, experiencing mild disease. She presented with five days of dyspnoea, fever, and cough. Antibiotics were initiated in primary care, but without benefit. Chest x-ray on admission revealed bilateral diffuse infiltrates. COVID-19 PCR was negative. A broad infectious work-up was negative: PCR for respiratory viruses, atypical bacteria and cytomegalovirus (CMV), legionella urinary antigen, cryptococcal antigen, galactomannan, and blood cultures. Treatment with ceftriaxone, levofloxacin, and hydrocortisone resulted in moderate clinical improvement, still requiring oxygen supplementation. Chest CT angiography ruled out pulmonary embolism but revealed GGO with subpleural dominance. She was discharged with oxygen supplementation but was readmitted the following day due to worsening of her clinical state. Treatment with trimethoprim/sulfamethoxazole, piperacillin/tazobactam, ganciclovir, and hydrocortisone was initiated. She continued to deteriorate, requiring intubation and transfer to the intensive care unit. BAL was negative for COVID-19 PCR, viral cultures, respiratory panel PCR , pneumocystis pneumonia, CMV, and galactomannan.
Patient 3
A 77-year-old woman with rheumatoid arthritis, treated with rituximab and vaccinated with BNT162b2 three times. She was diagnosed with COVID-19 a month prior to admission experiencing mild disease, and was considered convalescent three weeks prior to admission. Several days prior to admission she developed fever, cough, and weakness, with preserved saturation and a normal chest x-ray, and was treated with ceftriaxone, amoxicillin, and azithromycin. A few days later she was admitted due to symptom persistence. An admission chest x-ray revealed interstitial infiltrates. COVID-19 PCR was negative. Blood cultures, PCR for respiratory viruses, atypical bacteria and CMV, legionella urinary antigen, cryptococcal antigen, and galactomannan were negative. She continued to deteriorate clinically under treatment with ceftriaxone and levofloxacin. Treatment with hydrocortisone was initiated. Chest CT revealed GGO involving both lungs. BAL was negative for a wide array of infectious aetiologies, including respiratory virus panel PCR, pneumocystis pneumonia, CMV, and galactomannan. COVID-19 PCR from the BAL was not performed. She continued to deteriorate under trimethoprim and sulfamethoxazole, and piperacillin/tazobactam, eventually requiring intubation and transfer to the intensive care unit. Considering the possibility of organising pneumonia she was treated with pulse methylprednisolone, improved clinically, and was successfully extubated.
Patient 4
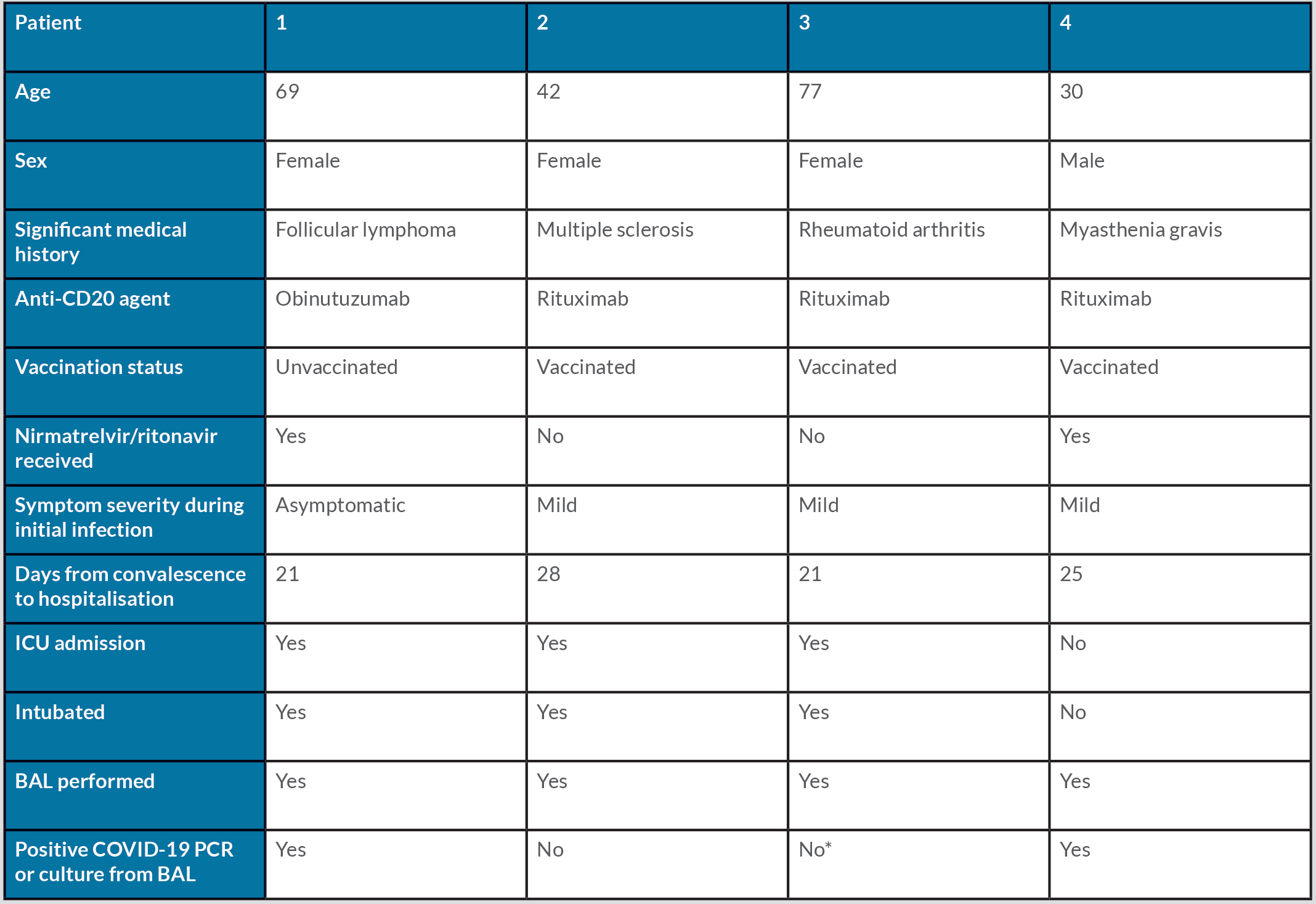
A 30-year-old man with a history of myasthenia gravis and eosinophilic granulomatosis with polyangiitis, treated with rituximab, and vaccinated with BNT162b2 three times. He was diagnosed with COVID-19 infection five weeks prior to admission, treated with nirmatrelvir/ritonavir and considered convalescent after ten days. Two weeks prior to admission he developed dyspnoea and fever, and was treated with oral corticosteroids. Symptoms persisted and he underwent chest CT imaging, revealing diffuse bilateral GGO. BAL was positive for COVID-19 PCR. He was admitted and received convalescent plasma, and was discharged in good clinical condition after several days (Table 1).
Table 1. Demographic characteristics, underlying disease and clinical presentation of four patients treated with anti-CD20 agents who developed late respiratory complications after convalescence from COVID-19.
* BAL was performed but COVID-19 was not tested.
DISCUSSION
We described a clinical syndrome affecting anti-CD20 treated patients: mild or asymptomatic initial COVID infection, a latent period lasting a few weeks followed by progressive respiratory deterioration, sometimes leading to respiratory failure. B cells have been shown to be important for an effective immune response against COVID infection [5], and thus their depletion undermines the immune system’s response. As such, a correlation between anti-CD20 treatment and severe COVID has been described [2]. However, a biphasic course has yet to be described. Possible explanations for this clinical course include persistent COVID or a late hyperimmune response. Treatment with nirmatrelvir/ritonavir, conferring transient protection against severe disease, may also play a role. All cases took place when Omicron was the prevalent variant, and so the clinical course described here might be unique to Omicron. Clinicians must be aware that COVID-related respiratory complications can appear in presumably convalescent anti-CD20 treated individuals weeks after mild infections. The convalescent status of these patients meant treatment by multiple antibiotics before COVID was considered. We hope that awareness of the possibility of a biphasic course as described will lead to quicker diagnosis, proper isolation, and more timely treatment, with rapid utilisation of BAL.