ABSTRACT
Takotsubo syndrome is known for its association with psychological stress factors. Rarely, it is associated with invasive procedures. We present a case of Takotsubo induced by bronchoscopy, a procedure with a low rate of complications.
LEARNING POINTS
- Takotsubo or stress cardiomyopathy is associated with physical and psychological stress factors.
- Takotsubo syndrome (TS) associated with bronchoscopy is rare.
- TS should be included in the differential diagnosis of both female and male patients.
KEYWORDS
Takotsubo, bronchoscopy, cardiomyopathy, magnetic resonance imaging
INTRODUCTION
Takotsubo syndrome (TS) is characterized by transitory left ventricular dysfunction [1, 2]. The phenomenon tends to occur among postmenopausal women and is marked by anginous precordial pain and electrophysiological parameters seen in acute myocardial infarction. Dyskinesis or akinesis of the anterior wall of the left ventricle due to ballooning of the apex contrasted with increased activity of the ventricular base is seen on echocardiogram. As regards aetiology, TS does not have a clear pathophysiological mechanism but seems to be associated with physical or psychological stressors. Although occasionally occurring due to invasive procedures, TS associated with bronchoscopy is rare.
CASE DESCRIPTION
A 61-year-old male patient with a history of type 2 diabetes, dyslipidaemia, hyperuricaemia and rheumatic disease presented to the emergency department with a 7-day history of fever, fatigue and headache. On admission, oxygen saturation was 82%, serum lactate dehydrogenase (LDH) was 4.5 mmol/l, C-reactive protein (CRP) was 45.6 mg/l, D-dimer was 1.268 µg/l and lymphopenia was present. A computed tomography scan of the chest showed bilateral diffuse ground-glass opacities, while a transthoracic echocardiogram demonstrated concentric remodelling, impaired relaxation of the left ventricle, minimal aortic and mitral regurgitation, and an ejection fraction of 66%. Seven reverse transcriptase quantitative polymerase chain reaction (RT-qPCR) tests on nasopharyngeal samples were negative for SARS-CoV-2. As a result, it was decided to perform bronchofibroscopy to collect bronchoalveolar washes for culture and investigation of other viruses.
After bronchoscopy, the patient presented acute respiratory distress, hypotension, tachycardia, hypoxaemia and then slurred speech. Supportive measures were undertaken, resulting in progressive improvement.
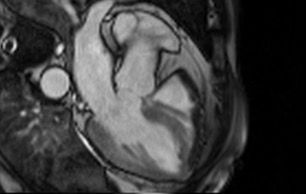
The patient returned for follow-up tests the next day, without symptoms but with an elevated CRP of 107.7 mg/l and a serum troponin of 3,091.6 pg/ml. Cardiac magnetic resonance imaging showed akinesia in the middle segment of the anterior, lateral and inferior walls, preserved contractility, and a left ventricle ejection fraction of 49%, which suggested TS (Fig. 1 and Vid. 1). Further angiographic investigation 8 days later revealed no obstructive pathologies of the coronary arteries. The patient was discharged the following day and transferred to outpatient services.
Figure 1. Myocardial magnetic resonance image showing ballooning of the ventricular apex
Video 1. Akinesia in the middle segment of the anterior, lateral and inferior walls, preserved contractility, and a left ventricle ejection fraction of 49%.
DISCUSSION
Takotsubo or stress cardiomyopathy is a syndrome characterized by transitory regional systolic dysfunction, occurring primarily in the left ventricle, mimicking an acute myocardial infarction without presenting angiographic findings of coronary artery obstruction caused by plaque destabilization. First described by Hiraku Sato in 1990, the term takotsubo refers to the Japanese name for a trap used to catch octopus, which systolic left ventricular apical ballooning resembles during stress cardiomyopathy. The exact physiopathology of TS is uncertain, but an association with catecholamine release due to excess stimulation of the sympathetic autonomic nervous system [3, 5]has been reported in cases of intense stress and iatrogenic administration of catecholamines [4, 5, 8]. TS is more frequent in older women, probably due to increased myocardial susceptibility to sympathetic stimuli [6].
In the reported case, the development of TS was preceded by bronchoscopy, a normally safe procedure that is a diagnostic and therapeutic pillar of pulmonary medicine. Complications of bronchoscopy are uncommon and usually occur in older patients with coexisting coronary artery disease, hypertension or compromised pulmonary function, with most of these events being hypoxaemia, arrythmias, bleeding, pneumothorax and pneumomediastinum [9, 10].
A typical case of TS is characterized by anginous precordial pain and electrophysiological anomalies, such as ST segment elevation or T wave inversion, which facilitates underdiagnosis due to low clinical suspicion [3, 4]. Imaging studies are essential for establishing a diagnosis of stress cardiomyopathy, especially coronary angiography and myocardial magnetic resonance imaging. Transthoracic ultrasound is also being employed as a possible diagnostic test, showing dyskinesia or akinesia on the anterior wall of the left ventricle due to ballooning of the ventricular apex [6, 9]. Although significant, such anomalies of ventricular function are self-limiting and tend to resolve spontaneously [3, 9].
As TS can be a challenging diagnosis, this case shows that although it tends to affect female patients, it must also be a differential diagnosis for male patients. Moreover, TS after bronchoscopy demonstrates that relatively safe invasive procedures can also provoke stress cardiomyopathy.