ABSTRACT
Intraocular lymphoma (IOL) is a rare and life-threatening condition whose aetiology is unclear. Blurred vision, reduced vision, and floaters are common initial symptoms. Posterior vitreous detachment and haemorrhage rarely occur.
The authors present the case of a 79-year-old man who initially presented with a 3-month history of fever, night sweats, significant weight loss, bilateral peri-orbital haematoma, red eyes and retro-orbital headache. Physical examination revealed fever, bilateral peri-orbital haematoma, subconjunctival haemorrhage and palpable cervical lymphadenopathy. CT scans detected conical intra-orbital lesions, cervical adenomegalies, expansive lesions in the adrenal glands, and thrombosis of the splenomesenteric confluent and posterior segment of the right branch of the portal vein. These findings were suggestive of a lymphoproliferative disorder. Aspiration cytology of the adrenal mass and inguinal adenopathies was compatible with diffuse large B-cell lymphoma with areas of transformation to Burkitt’s lymphoma.
We describe a rare form of lymphoma, and a very unusual presentation of primary intraocular lymphoma with atypical symptoms.
LEARNING POINTS
- Intraocular lymphoma is a rare disease and can mimic common infectious or non-infectious uveitis.
- Bleeding or periocular haematoma are suggestive of intraocular lymphoma.
KEYWORDS
Intraocular lymphoma, ocular haemorrhage, adrenal mass
INTRODUCTION
Intraocular lymphoma (IOL) is a life-threatening condition which results from one of two types of a rare lymphocytic malignancy: primary intraocular lymphoma (PIOL) and secondary intraocular lymphoma (SIOL) [1–3]. The former is mainly a subtype of primary central nervous system lymphoma (PCNSL) [1, 2, 4, 5]. It can arise in the retina, uvea, vitreous [5] or optic nerve [1, 6]. By far the most common PIOL is primary vitreoretinal lymphoma (PVRL). IOL can also originate from outside the central nervous system (CNS) by metastasizing to the eye. These tumours are known as SIOL. The most common subtype of SIOL is systemic diffuse large B-cell lymphoma (DLBCL). Most cases have a B-cell origin [1, 4, 5], but there are also T-cell variants, which are very rarer.
The incidence of IOL has increased in recent years [1, 4]. There appears to be no racial [1, 5] or gender predilection. The aetiology remains unknown.
Diagnosis remains challenging and there is often misdiagnosis and delay [1, 5–7]. Therefore, it is important to keep in mind that ocular haematoma or subconjunctival bleeding may indicate intraocular disease.
Approximately one-third of PIOL patients have concurrent PCNSL at presentation and up to 92% will develop PCNSL within a mean of 8–29 months [5]. Tumour recurrence is common and sometimes treatment cannot prevent local recurrence and CNS involvement.
CASE DESCRIPTION
A 79-year-old man, with a medical history of atrial fibrillation for which he was taking warfarin, was admitted to hospital with a 3-month history of fever, night sweats, productive cough and significant weight loss, with no response to previous antibiotic regimens. He also referred the emergence of bilateral periorbital haematoma and subconjunctival haemorrhage associated with severe retro-orbital headache. There was no history of trauma or other reported symptoms.
Physical examination showed pale mucous membranes, bilateral peri-orbital haematoma, subconjunctival haemorrhage, and deep centrimetric cervical adenopathies with a hard consistency.
Laboratory investigation showed bicytopenia with normochromic normocytic anaemia and thrombocytopenia, an International Normalized Ratio above the therapeutic range (INR 5.57), increased sedimentation rate (120 mm in the 1st hour), raised lactate dehydrogenase level (1098 IU/l) and elevated beta-2-microglobulin (5.85 mg/l).
Infectious diseases were ruled out by serology studies, and blood and sputum bacterial and mycobacterial culture. Autoimmunity tests were negative.
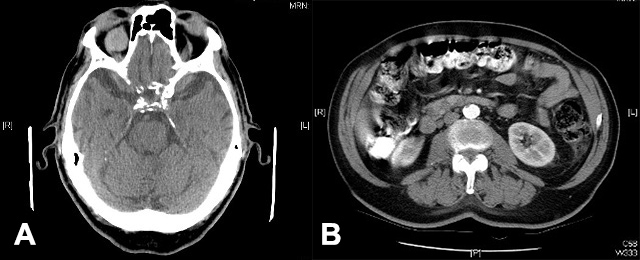
To investigate the non-traumatic peri-orbital haematoma, subconjunctival haemorrhage and severe retro-orbital headache, brain and orbit computed tomography (CT) scans were performed and showed intra-conical intra-orbital lesions (Fig. 1a). A brain MRI indicated these lesions were highly suggestive of a lymphoproliferative disorder.
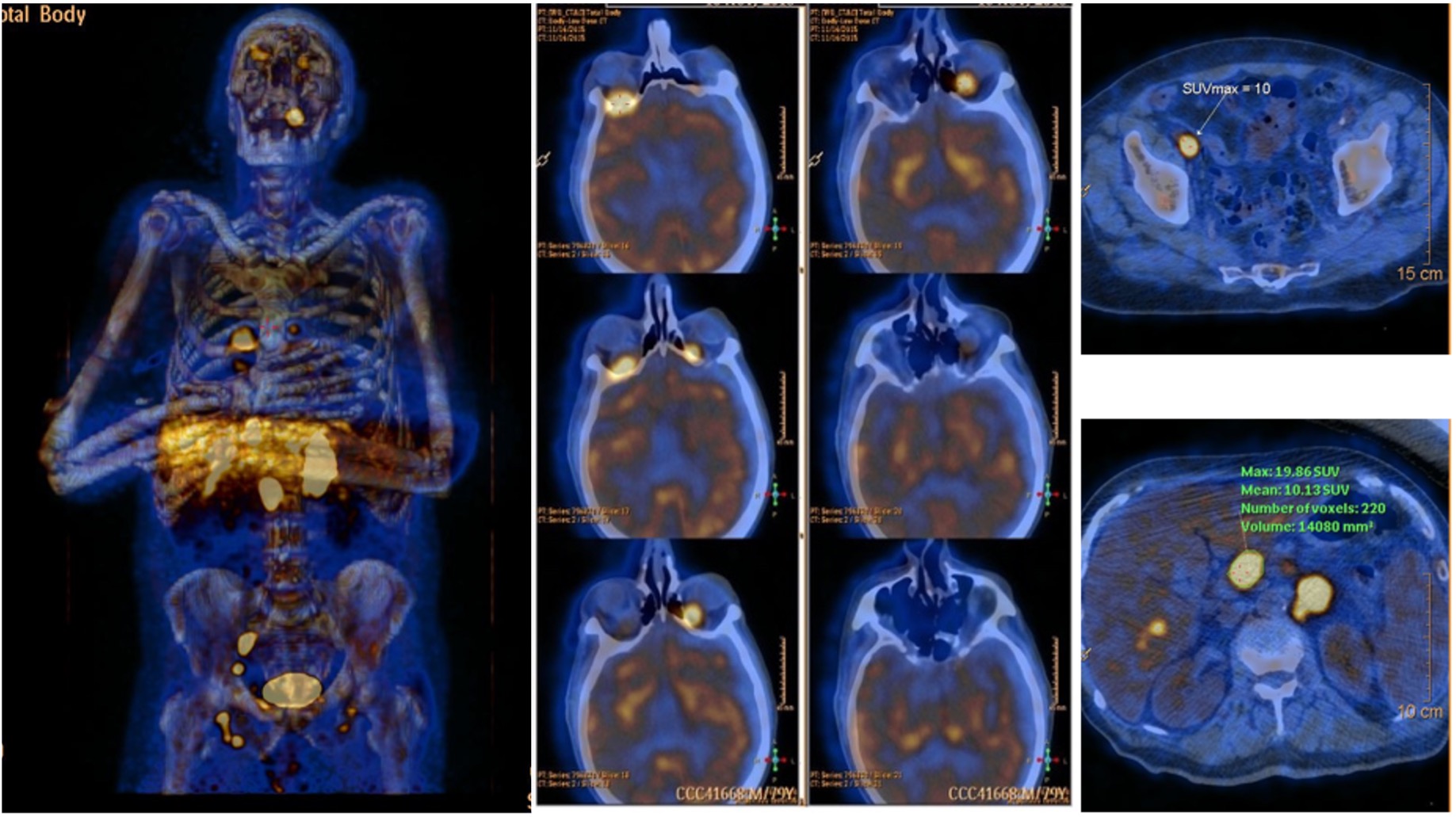
A body CT scan revealed cervical adenopathies, expansive lesions of the adrenal glands, and thrombosis of the splenomesenteric confluent and posterior segment of the right branch of the portal vein (Fig. 1b). Abdominal MRI was performed to clarify the CT findings but was inconclusive regarding the nature of the adrenal gland lesions. A positron emission tomography (PET) scan showed metabolically active disease at the bilateral intra-orbital, ganglionic, hepatic and bilateral adrenal levels (Fig. 2).
Figure 1. Full body CT scan showing cervical adenomegalies, expansive lesions in the adrenal glands, and thrombosis of the splenomesenteric arterynconfluent and posterior segment of the right branch of the portal vein
Figure 2 PET scan demonstrating metabolically active disease at the bilateral intra-orbital, ganglionic, hepatic and bilateral adrenal levels
DISCUSSION
The diagnosis of IOL requires a multidisciplinary approach. Although it has been reported that women are more commonly affected than men [3, 5, 8, 9] in their fifth to seventh decade of life, our patient was male and in his seventies.
Due to its rarity and ability to mimic other diseases [1, 3, 5], IOL requires a multidisciplinary approach involving traditional immunocytochemistry, morphological assessment and molecular analysis [5]. The differential diagnosis includes infections such as syphilis, tuberculosis, cytomegalovirus (CMV), HIV and toxoplasmosis, inflammatory diseases such as sarcoidosis, multiple sclerosis, pars planitis, other metastatic tumours, and idiopathic intermediate uveitis [3, 5, 10]. Consequently, our patient was extensively investigated.
The fever, night sweats, productive cough and significant weight loss suggested an infectious, inflammatory, autoimmune or neoplastic cause. Serology and autoimmune tests were negative. The brain CT scan indicated possible neoplastic disease so a brain MRI was performed to examine the intra-conical intra-orbital lesions and strongly suggested a lymphoproliferative disorder. MRI is more sensitive than CT for detecting lesions in the CNS, but both are limited for evaluating ophthalmic diseases [5]. The MRI indicated these lesions were highly suggestive of a lymphoproliferative disorder, so a body CT scan, an abdominal MRI and, lastly, a PET scan were performed.
Histological identification is essential for diagnosis [1, 4, 11], so it was only after cytological examination that the diagnosis was made.
IOL prognosis remains poor and depends on whether the CNS is involved, the histopathological type and treatment opportunity. The mortality rate ranges between 9% and 81% [1, 5]. In our case, despite the absence bone marrow and CNS involvement, the patient had a poor performance status and refused curative chemotherapy.
Intraocular disease was not suspected at first in this patient. The first investigations considered infectious diseases such as atypical pneumonia due to Mycoplasma pneumoniae and Legionella pneumophilia, tuberculosis, syphilis, CMV, HIV and toxoplasmosis, inflammatory and autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus, and neoplastic diseases such as lymphoma, leukaemia and CNS tumours. Only with imaging test results and histological identification did the diagnostic hypothesis of intraocular disease arise. Like many other cases in the literature, the diagnosis was delayed for almost 3 months.
Although IOL is still very rare, its incidence has increased so it is important to recognize the risk factors and signs suggestive of intraocular disease, such as bleeding or periocular haematoma. This condition merits further investigation in order to improve outcomes.