ABSTRACT
Introduction: Non-episodic angioedema associated with eosinophilia (NEAE) has been reported primarily in young East Asian women and is characterized by a single episode of persistent limb oedema, peripheral eosinophilia, and transient joint pain. Although there are reports of eosinophilia disease after coronavirus disease 2019 (COVID-19), the occurrence of NEAE has not been previously reported.
Case description: A 29-year-old Japanese woman, with a history of allergic rhinitis and atopic dermatitis, sought a medical consultation for persisting oedema of the extremities, which developed about 2 weeks after she contracted COVID-19. Physical examination revealed symmetrical non-pitting oedema with peripheral predominance. Laboratory examination revealed a blood eosinophil count of 7536/µl. The patient was diagnosed with NEAE and a 7-day course of prednisolone (15 mg/day) was initiated, with rapid improvement in the oedema and no recurrence on follow-up.
Discussion: The exact aetiology of NEAE is unknown, but it may develop after infection or drug exposure. Eosinophilic disease after COVID-19 infection has been reported and, therefore, eosinophilic angioedema should be considered in the differential diagnosis of non-pitting oedema of the extremities after a COVID-19 infection. Early diagnosis of NEAE is important as rapid improvement can be achieved with low-dose steroid treatment.
Conclusion: NEAE can develop after COVID-19 and should be considered in the differential diagnosis of non-pitting oedema of the extremities.
LEARNING POINTS
- Non-episodic angioedema associated with eosinophilia (NEAE) is characterized by a single episode of symmetrical non-pitting oedema with distal limb predominance.
- The case presented indicates that NEAE can occur after COVID-19 infection.
- Serum IgA levels may be helpful to identify TA patients not responding to traditional therapy.
KEYWORDS
COVID-19, non-episodic angioedema with eosinophilia, non-pitting oedema
INTRODUCTION
There are two types of angioedema with eosinophilia: episodic angioedema with eosinophilia (EAE), also known as Gleich syndrome, and non-episodic angioedema associated with eosinophilia (NEAE). EAE has been reported mainly in Europe and the USA and is characterized by angioedema, urticaria, fever, recurrent oedema, and a marked increase in peripheral blood eosinophil count and serum IgM levels. NEAE, on the other hand, has been reported mainly among young East Asian women and is characterized by a single episode of persistent oedema of the extremities, peripheral eosinophilia, and transient arthralgia, with no increase in serum IgM levels and a milder clinical course than EAE [1, 2].
Although the detailed pathogenesis of NEAE is not yet known, it can occur after infection or drug exposure [3]. Herein, we report a case of NEAE after coronavirus disease 2019 (COVID-19) infection. To our knowledge, while there have been reports of various autoimmune diseases after COVID-19, the occurrence of NEAE has not been previously described.
CASE DESCRIPTION
A 29-year-old Japanese woman, with a history of allergic rhinitis and atopic dermatitis, presented to our office with a history of oedema of the extremities over a period of 2–3 weeks prior to the consultation. She had contracted COVID-19 approximately 1 month previously and had been recuperating at home for 10 days. Immediately after the recuperation period, she noticed swelling of both lower extremities, 17 days before the visit, and swelling of both hands, 13 days before the visit. She sought initial treatment at a local clinic and was prescribed Chinese herbal medicine with diuretic properties, with no improvement in her symptoms. There was no history of use of other medications, supplements or over-the-counter drugs.
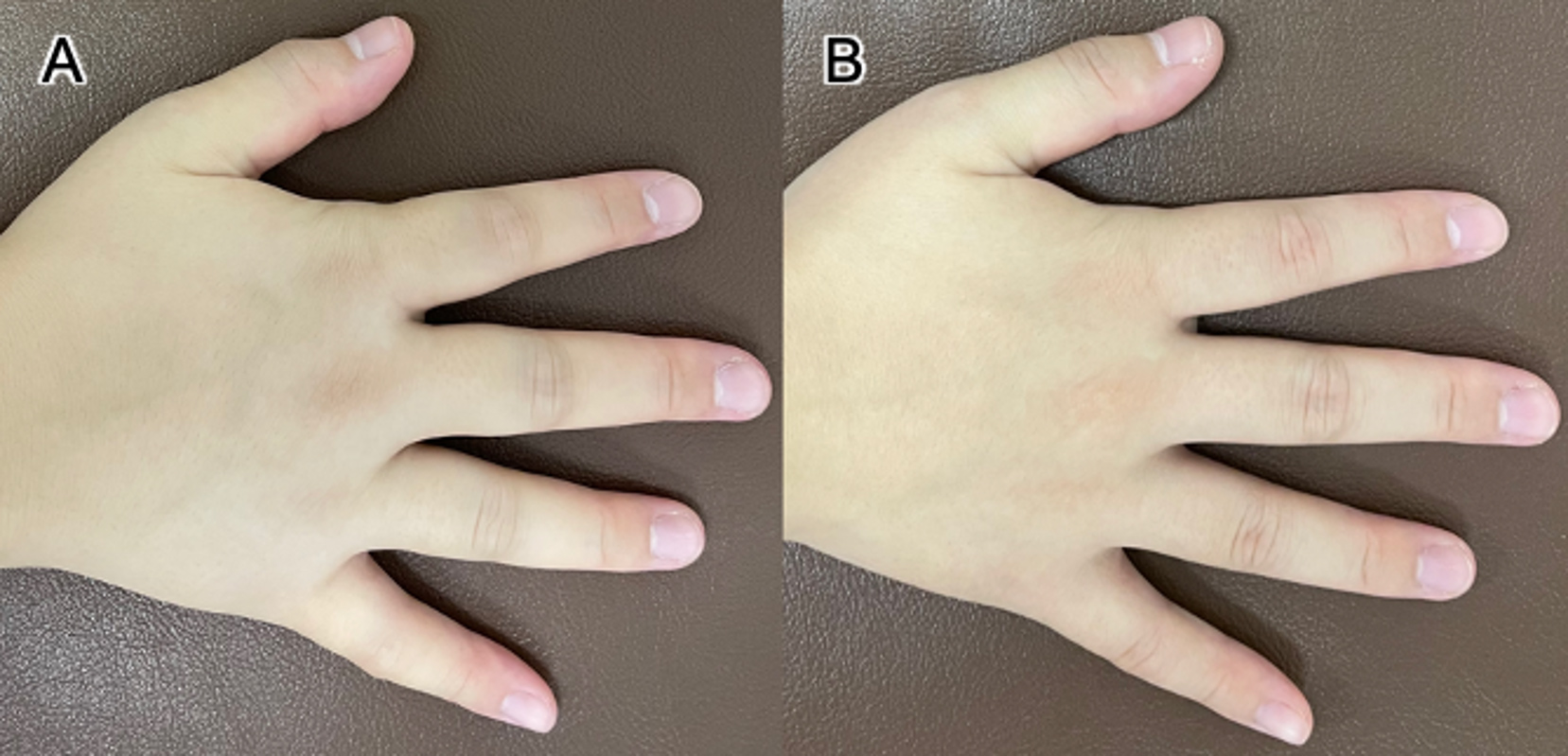
The physical examination revealed symmetrical non-pitting oedema, with distal limb predominance (Fig. 1). Laboratory tests revealed blood eosinophilia (7536/μl), with no abnormalities in other laboratory results, such as thyroid function, and a negative pregnancy test.
Figure 1 (A) The patient's right hand before treatment, with reduced finger wrinkles especially in the proximal interphalangeal joint area of the index finger due to non-pitting oedema. (B) After treatment, the finger wrinkles returned to normal
NEAE was diagnosed and a 7-day course of prednisolone (15 mg/day) prescribed. Improvement in the oedema in her hands was observed on treatment day 1 and in her feet on day 3. The patient completed the 7-day course of prednisolone. There was no recurrence of oedema on follow-up.
DISCUSSION
Our case describes the occurrence of NEAE after COVID-19 infection in a young Asian woman with a predisposition to allergy, where allergy is the predominant predisposing factor for NEAE. In the absence of a history of drug exposure and travel, COVID-19 was deemed to be the primary aetiological cause of NEAE in this case. To the best of our knowledge, this is the first report of NEAE after COVID-19.
Although the exact pathogenesis of NEAE is unknown, the fact that it is more common among women and occurs after infection or drug exposure suggests that NEAE is the result of an abnormal immune response to various exogenous stimuli in genetically susceptible individuals, with sex hormones likely playing a role [3]. Eosinophilic disease after COVID-19 infection has been reported, namely eosinophilic pneumonia and eosinophilic granulomatosis with polyangiitis [4, 5]. In addition, there have been reports of NEAE after vaccination against SARS-CoV-2 [6]. At this time, there is no clear link between COVID-19 and autoimmune diseases; however, since the protein of SARS-CoV-2 shows some similarities with human proteins, destruction of the autopeptide may lead to autoimmunity [7]. There are also reports of post-COVID-19 onset of angioedema, an oedematous disease with a similar mechanism that causes bradykinin-induced oedema of the skin, airways, gastrointestinal tract, and other organs [8, 9]. Dysregulation of the angiotensin-converting enzyme 2 receptor, which is the entry point for the SARS-COV-2 virus, and racial factors have also been considered in the pathogenesis of angioedema. Racial differences in the epidemiology of NEAE and EAE have also been noted; thus, race may also be a factor worth investigating [2, 10].
Non-pitting oedema was observed in our patient, which is consistent with previous reports on NEAE [2, 6, 11]. The principal differential diagnoses of non-pitting oedema with distal limb predominance are lymphoedema and thyroid dysfunction [12], with NEAE also having been reported [2, 6, 11]. As NEAE is a non-fatal and self-limiting disease which improves rapidly with low-dose steroids, early and accurate diagnosis is important to prevent unnecessary visits and tests [13].
CONCLUSION
In summary, we present a case of NEAE as a rare complication after COVID-19. Based on our experience, we suggest that eosinophilic angioedema, including EAE and NEAE, should be considered in the differential diagnosis of non-pitting oedema of the extremities, in addition to thyroid disease and lymphoedema.